Cancer's 'Achilles' heel' discovered by British scientists raising hope of 'cure'
Findings mean each patient 'would have a unique, bespoke treatment' that marshals immune cells to exploit the weakness identified
A major British discovery is expected to lead to revolutionary bespoke treatments for patients with advanced cancer that could enter trials within two years.
The scientists behind the breakthrough believe they have identified the “Achilles’ heel” of cancer cells.
In a video about the findings, Cancer Research UK, described how immune cells could be marshalled to exploit this weakness.
“They could form a fierce cancer-fighting force with the potential to target every cancer cell in the body,” the video said. The research could even result in “a revolutionary way to treat or even cure cancer”, the video added.
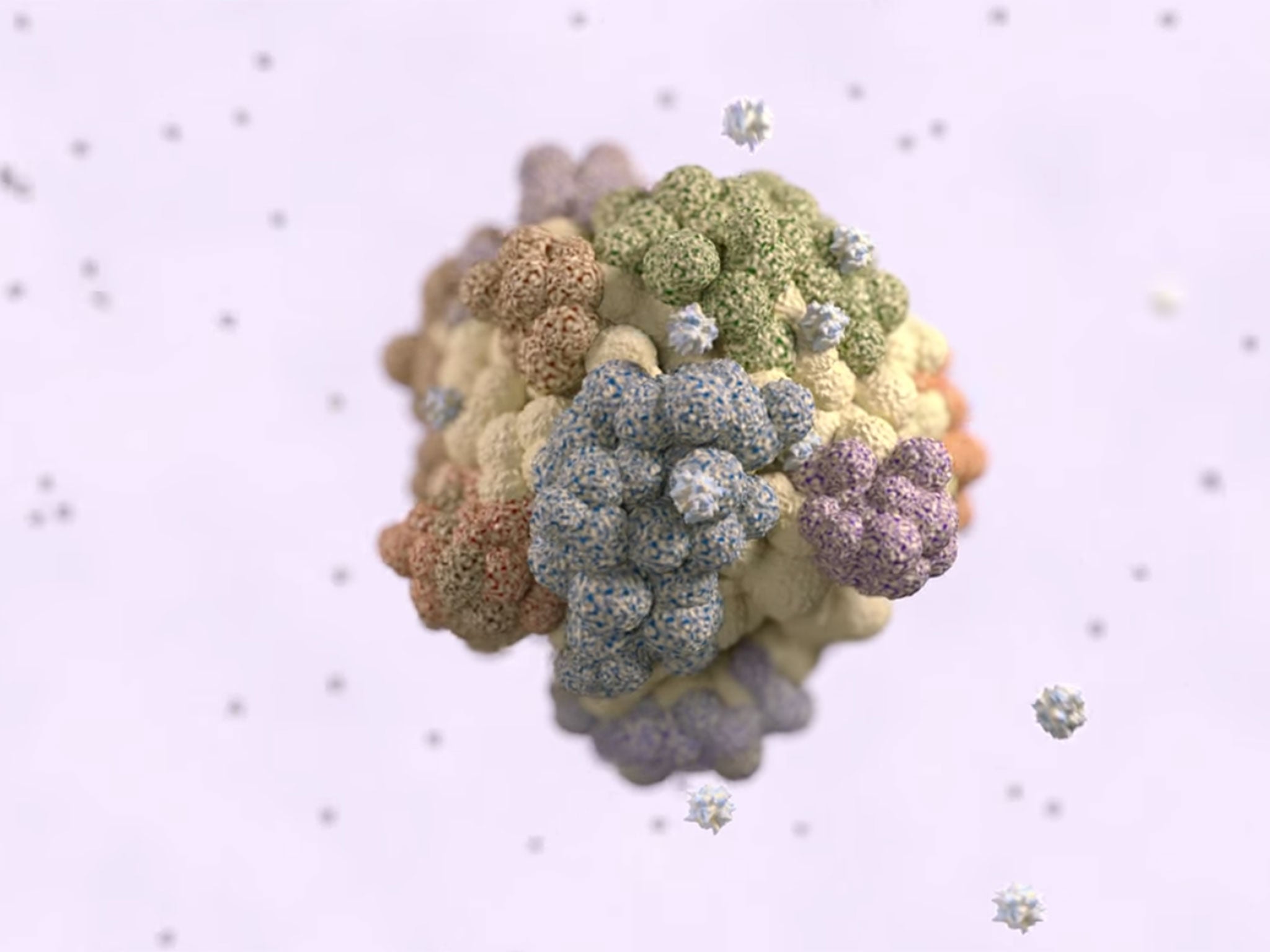
The researchers found rare "flag" proteins that act as immune system targets and are displayed on the surface of all of a patient's tumour cells, wherever they might be in the body.
Normally they are shielded from the immune system, or missed because rapidly evolving cancers present too many constantly changing targets.
Once the omnipresent proteins, or "antigens", are isolated, potent immune system cells called T-cells can be employed as homing missiles to zero in on them and destroy the cancer.
Such an approach, which involves mapping the DNA in a patient's tumour sample, would help to overcome the ability of cancers to resist therapies by altering their genetic make-up.
The work is at an early stage and so far just two of the special antigens, plus the T-cells that recognise them, have been identified in two lung cancer patients.
But the scientists hope to see rapid progress leading to patient trials, and are optimistic about similar targets for other cancers being found.
Professor Charles Swanton, from University College London's Cancer Institute, a leading member of the Cancer Research UK-funded team, said: "I will be disappointed if we haven't treated a patient within two years.
"Do we think it's going to work? I hope this is going to result in improvements in survival outcomes. If this doesn't work, I'll probably hang my hat up and do something else."
He pointed out that a tumour evolutionary tree was like a "snowflake or fingerprint", unique to each patient. That presented a problem for clinicians and patients, because as tumours developed the tree grew new branches containing novel genetic mutations which helped the cancer resist treatment.
The new research had shown there were potential immunotherapy targets from the "trunk" of the tree that are flagged up on all of a tumour's multiplying cells.
Prof Swanton added: "This is exciting... now we can prioritise and target tumour antigens that are present in every cell, the Achilles’ heel of these highly complex cancers.
"This is really fascinating and takes personalised medicine to its absolute limit, where each patient would have a unique, bespoke treatment."

One way of exploiting the discovery would be to develop T-cell-activating vaccines based on the antigens, said the researchers, whose findings are reported in the journal Science.
Another would be to "fish out" the small number of T-cells in tumours that are naturally primed to recognise the antigens, multiplying them in a laboratory, and returning them to the patient.
Currently there are too few of the ready-primed T-cells in patients to make a difference. In the samples analysed by the scientists, they only made up 1% to 2% of the T-cells in a tumour.
Another hurdle to be crossed is the way cancer protects itself using proteins that are normally employed to keep the immune system in check and prevent it running out of control.
In practice, the new antigen-targeting therapies would have to be accompanied by so-called "checkpoint inhibitors" - drugs that are already being used to treat cancer patients.
Professor Peter Johnson, Cancer Research UK's chief clinician, said: "This ... research gives us vital clues about how to specifically tailor treatment for a patient using their immune system.
"It gets us closer to knowing why some patients respond to immunotherapy treatment and others don't, and how we might select which patients will benefit the most."
The research was also funded by the Rosetrees Trust, set up in 1987 to support life-changing medical science.
Experts are increasingly coming round to the idea that the future of cancer treatment is personalised medicine, tailored to small groups of patients or even individuals.
A new more effective approach to tackling cancer is desperately needed, Prof Swanton believes.
He said 71 new anti-cancer drugs approved by the US Food and Drug Administration (FDA) over a period of 12 months were associated with a typical survival time of no more than two months.
On average, each course of treatment cost 100,000 dollars (£70,727).
Prof Swanton added: "This is the emperor of all maladies. It's just a massive challenge, because this disease is unlike all other diseases that we see in medicine. We're dealing with an entity that's constantly evolving, constantly adapting, and constantly changing its genome."
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks