Drug-resistant cancers kill millions – here’s how we're tackling them
Tumour evolution was first identified 40 years ago. We're finally making good progress with it
Cancer treatment is often highly effective at first, yet patients’ tumours can stop responding even to the most advanced therapies. Sometimes in cases where the patient has gone into remission and the cancer has apparently been thwarted, it can return and no longer respond to treatment. In both cases, this is because the cancer cells evolve.
Most of us are familiar with Darwinian evolution, whereby individual traits that are advantageous in an environment tend to survive to become dominant features in a species. In the 1970s, the American cancer researcher Peter Nowell established that a similar thing happens with cancer.
Trying to overcome this problem is one of the key frontiers in 21st century cancer research. The good news is that the progress looks promising.
How cancers evolve
Cancers often arise because the genes responsible for repairing DNA, and the genes that kill off cells with badly damaged DNA, become damaged themselves. This creates an environment where cancerous mutations in DNA are not repaired or removed and are allowed to accumulate. Not only does this allow tumours to grow in the first place, it also means they are more able to adapt and evolve to become drug-resistant – creating a vicious circle.
Treatments themselves can also act as a selective pressure that drives cancer cells to evolve. To take an example from prostate cancer, which is my research area, tumours are very responsive to being deprived of testosterone since they usually depend on the hormone to grow in their early stages. In some cases, however, the disease becomes resistant to this treatment.
Normally, the body needs testosterone to activate the receptors responsible for switching on genes that direct male sexual characteristics and certain other traits, including the growth of the prostate tissue. But where, for example, there are mutations to the gene that encodes this receptor, it can enable the receptor to be activated by other molecules.
In such circumstances, lowering a patient’s testosterone level will no longer act as a block on the growth of the cancer cells. This is known as castrate-resistant prostate cancer. Where it has spread to produce secondary tumours (metastasis), this highly aggressive form of the disease is considered incurable.

Resistance mechanisms have also been well documented in response to radiotherapy and chemotherapy. In chemotherapy, for example, drug resistance is said to be responsible for 90 per cent of treatment failures where there are secondary tumours.
A particularly problematic resistance mechanism is one where in response to certain treatments, cancer cells actually change their cell type from those which make up the majority of most organs (epithelial), to cells more involved in hormonal and nerve signalling (neuroendocrine cells).
Known as neuroendocrine differentiation, the changed cells are resistant to chemotherapy and radiation treatment. This has been observed with prostate, lung and colorectal cancers, and no drug currently exists to specifically target the process.
Personalised medicine
So how can we overcome the challenge presented by tumour evolution? Peter Nowell recognised in 1976 that this would necessitate “individual specific therapy”. Forty years later, the age of personalised medicine that this pre-empted is now well underway.
The first cancer treatment to specifically target the effects of tumour evolution was Herceptin, which was originally approved for clinical use in the late 1990s. Herceptin is a drug that specifically targets a protein called HER2, which is a key driver of some breast cancers. It is considered an individual therapy because HER2 levels are particularly high in about 20-30 per cent of breast cancers; and was the first of a class of what are known as molecular-targeted cancer therapies
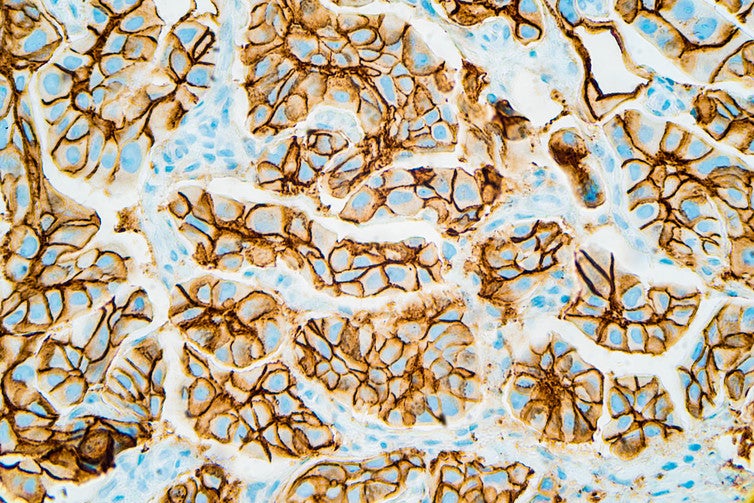
Herceptin works by sticking to HER2, which prevents the protein from causing cancer growth. Unfortunately, of those who respond well to the drug, around 70 per cent will still progress to the metastatic stage within a year of treatment.
The problem is that the drug is often neutralised itself by tumour evolution, in this case from mutations to HER2 “cutting off” the part that Herceptin needs to stick to. In addition, sometimes levels of another protein called HER3 increase to compensate for the loss of effective HER2. HER3 can itself drive cancer growth and Herceptin is unable to stick to it.
These two examples of Herceptin resistance are typical of how cancer cells operate: they can both benefit from direct mutations to their DNA (in this case in relation to HER2), but also to influence which genes are “switched on or off” (in this case switching on HER3). We describe these as epigenetic changes, meaning they are “above genetics”.
To overcome these difficulties, cancer research has had to look elsewhere. One exciting new approach involves predicting the course of an individual’s tumour evolution by analysing tumour DNA circulating in the blood.

These “liquid biopsies” make it possible to monitor how a patient is responding to a treatment in real time and to detect at an extremely early stage when cancers are either asserting themselves or “coming back”. We have recently seen promising results in relation to early-stage tumour evolution in lung cancer, for instance.
Also promising is immunotherapy, including a new treatment for prostate cancer sufferers called Provenge. It works by reprogramming the patient’s immune system by taking a specific type of immune cell out of their body and incubating it with a protein that is typically found on the surface of prostate cancer cells. When the cells are returned to the body, they can effectively “teach” the body how to attack its own tumour.
Though Provenge is not a cure for the metastatic castrate-resistant prostate cancer that I mentioned earlier, it does extend patients’ survival time by about 25 per cent, and the side effects are milder than chemotherapy and radiotherapy.
Other immunotherapy treatments in development are similarly geared towards extending survival times rather than “cure”. They are viewed within cancer research as the biggest breakthrough to have made it past clinical trials and be approved as treatments.
As our knowledge of specific kinds of tumour evolution in different cancers continues to progress, personalised treatment strategies like these are likely to become increasingly common. The costs will probably significantly decrease in parallel, which will take them mainstream – at present, for instance, Provenge has been deemed too expensive for use on the NHS.
We are talking about no less than a revolution in cancer therapy in the coming decades. Cancer survival rates have already more than doubled over the last 40 years from 24 to 50 per cent of all diagnoses in the UK. If the promise of personalised therapies bears out, there is every reason to expect those cancer survival rates to keep on climbing.
Joe Sutton is a PhD researcher in molecular biology at Edinburgh Napier University. This article was originally published on The Conversation (www.conversation.com)
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments