The Big Question: What are polyclinics, and why are doctors so angry about them?
The row over polyclinics reached a climax yesterday, with two separate developments
Why are we asking this now?
The row over polyclinics reached a climax yesterday, with two separate developments. While the British Medical Association stepped up the pressure on the Government by handing in a petition to No 10 against polyclinics signed by 1.2 million patients, a meeting of all 31 primary care trusts in London agreed to go ahead with plans for at least 150 polyclinics in the capital, as recommended in last year's report from the Health Minister Lord Ara Darzi. The Government also wants a network of "GP-led health centres" across the country.
Why are polyclinics such a hot potato?
Few would have predicted when Lord Darzi published his report a year ago that polyclinics would become a flashpoint between the Government, the profession and the Opposition. The BMA, having suffered one bloody nose at the hands of ministers last February over extended opening hours, resolved they were not going to suffer a second over polyclinics. They have mounted a successful "save our surgeries" campaign, claiming that ministers are bent on privatising general practice by bringing in commercial organisations. Ministers have responded by accusing the BMA of a "mendacious" campaign, deliberately misleading patients and spreading fear and despondency. The Tories say ministers' pledge that polyclinics will be in addition to existing GP services, rather than replacing them, will add £1.4bn to the NHS budget, over five times more than the £250m allocated.
What does this mean for the future of the NHS?
It looks bleak. Lord Darzi's review of the next stage of the NHS reforms is expected at the end of this month. From the beginning, he has stressed that progress depends on the involvement and co-operation of the medical profession and that the failure to recognise this has hampered progress in the past. Meanwhile, his fellow ministers and the BMA have been engaged in a slanging match the like of which has not been seen since Kenneth Clarke, the then Tory Health Secretary, accused BMA negotiators of "feeling for their wallets" 20 years ago. Relations between government and profession have reached a nadir.
What are polyclinics?
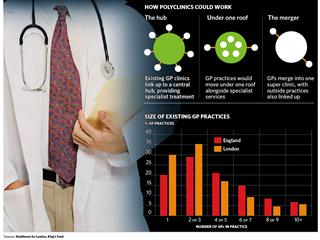
Not necessarily a single building – which has caused much confusion. The term may refer to a network of GP practices forming a "virtual" polyclinic. Essentially they are super-surgeries with up to 25 GPs, which will provide some hospital services such as X-rays, minor surgery and out-patient treatment. The simplest model involves several practices under one roof, sharing many services but operating as distinct practices with their own registers of patients (each of whom would have their own doctor). They would also offer consultations to patients not registered who walked in off the street, like existing NHS walk-in centres. A second, virtual model would involve a network of GP practices remaining in their own buildings but be linked to a local referral centre, which would provide diagnostic tests and outpatient clinics, either in a separate building or in one of the GP practices.
Why do the government and doctors disagree?
It is hard to say, because both sides keep shifting their ground. The BMA says polyclinics will mean patients have to travel further and undermine the personal relationship between patient and family doctor. Yet health centres containing a similar number of GPs have been part of the medical landscape for at least 30 years. The Government says polyclinics will be more convenient for patients, offering longer opening hours (8am to 8pm), and more services so they won't have to travel to hospital for tests and treatment. But despite ministerial denials of any diktat from the centre about their number, funding arrangements imply that every primary care trust must have at least one polyclinic or risk losing cash.
What is the case for polyclinics?
For decades, governments have talked about moving some care out of hospitals into the community, where it is more convenient for patients, reduces the burden on the hospitals and helps bridge the divide between primary and secondary care. None have succeeded, and staff numbers are growing faster in hospitals than in general practice, worsening the imbalance. Polyclinics are an attempt to solve this problem, and most experts welcome them as a suitable model for major cities, where hospitals are overwhelmed with minor cases and public transport is readily available.
What is the case against them?
A one-size-fits-all policy, which imposed polyclinics across the country, could do irreparable damage by driving out smaller local practices. They are not suitable for rural areas, where concentrating GPs in one place could create serious problems of access – though a virtual polyclinic might still work. A report by the Kings Fund last week, which examined the experience of other countries, found there was no evidence that polyclinics would improve care or save costs, even though they were able to provide a wider range of services.
What about the role of the private sector?
This is a crucial, unresolved issue. Primary Care Trusts will go out to tender for polyclinics, and commercial organisations such as United Health, Boots and BUPA will be able to bid against GPs for contracts to build and run them. The BMA says this is part of the Government's plan to "break" NHS general practice. Ministers say the private sector is essential to provide a competitive edge and to ensure services are geared to the needs of patients. Given the financial and management challenge involved in running a multi-million pound clinic with scores of staff, the dice may be weighted in favour of the biggest players. If that happens, commercial operators could focus on short-term contracts with a high turnover of staff and a loss of continuity of care for patients.
Who is to blame for this debacle?
The BMA bears a share of responsibility for its stubborn refusal to accept that there is anything wrong with general practice. While patients express themselves largely satisfied with what goes on in the consulting room, there is greater concern over what happens front of house – with access, appointments, and getting through on the phone. But ministers, too, must carry the can for failing to spell out their plans clearly and for ramping up the temperature of the debate with the profession. Now that polyclinics in London have got the go-ahead, a bout of bridge building is urgently needed between the two sides.
Will polyclinics be good for patients?
Yes...
*They will be more convenient for patients who need blood tests, investigations or outpatient treatment
*They will reduce the burden of routine work on busy inner-city hospitals, leaving them to concentrate on complex cases
*They will provide a boost to general practice, giving it more clout in the battle for resources with hospitals
No...
*Patients will have further to travel to receive a consultation and treatment from their GP
*Competition from polyclinics could draw patients away from local practices, forcing them to close
*Private commercial organisations will be better placed to bid for and run them, potentially undermining the NHS
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies