Care watchdog developing plans to use undercover surveillance to identify abuse of patients
Chief inspector says ministers must take responsibility as well as regulator
The care regulator could start using undercover surveillance to help identify where patients with a learning disability in care are being abused or neglected.
The Care Quality Commission has said it is drawing up plans on how it could use surveillance as part of a series of reforms to improve the watchdog’s ability to expose failing providers who fail to care for patients with learning disabilities and mental health needs.
It has also said it will increase the frequency of out of hours inspections in order to penetrate what it called “closed cultures” in some hospitals.
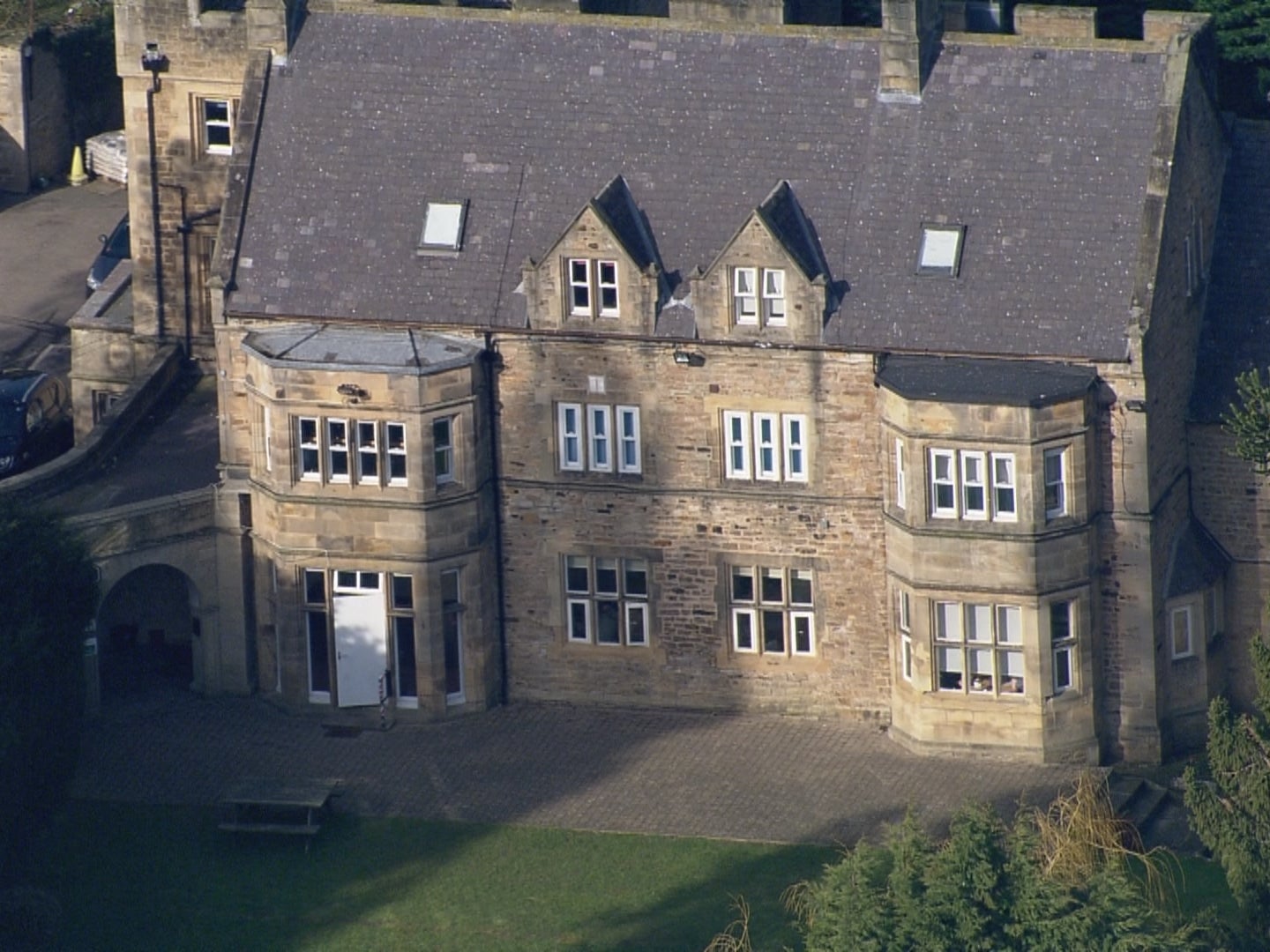
The changes are part of the regulator’s response to criticisms after it failed to identify abuse of patients at the private Whorlton Hall Hospital in County Durham.
An undercover BBC investigation in 2019 revealed widespread abuse of patients at the 17-bed hospital.
Following an independent report for the CQC by Professor Glynis Murphy the regulator which warned it had become to process driven, the watchdog has trained 2,000 inspectors on how to better understand whether a hospital has a bad culture.
In a new report for the regulator published earlier this week Professor Murphy said the CQC was unlikely to see evidence itself of abuse on inspections and referred to the recent case of a hospital in Essex where abuse was captured by the hospital’s CCTV.
She said: “This means that CQC must consider analysis of provider’s and family member’s video evidence, if they are to keep people safe from abuse.”
She added: “CQC needs to consider whether it also needs to instigate surveillance itself, for the rare occasions where there seems no other way to ensure people are safe.”
The CQC’s chief inspector of adult social care, Kate Terroni, told The Independent the watchdog was planning to go further and was looking at how it could gather evidence.
She said: “We are exploring the best way to make use of the surveillance powers that we have. We already use surveillance material sent to us by families and surveillance that a provider may have themselves, as well as information gathered by CQC inspectors through observations on visits.
“In the future, we may look at developing guidelines for when we might consider gathering information using overt or covert surveillance. However, we will not be making significant changes to our surveillance approach without engaging with providers and people who use services.”
She added the watchdog already carried out unannounced inspections out of hours and at weekends but would be “working to increase the number of these, especially in services at higher risk of developing poor cultures.”
Professor Murphy said the CQC had made progress since her first report but she also made new recommendations.
These include not rating a hospital as good or outstanding if it cannot demonstrate how the service supports whistleblowing and handles concerns being raised. She also said the regulator needed to consider how the use of restraint and segregation for people with learning disabilities should affect a service’s overall rating.
Other proposals included a tool to try and evaluate the culture of service and a bid to understand what life was like for people living in the hospital or care home.
In a blog post Kate Terroni said the CQC would continue working on the changes that were needed but she emphasised regulation alone was not the answer.
She said: “Regulation has a part to play in improving this, but we can’t do it alone. We need the rest of the system to take responsibility too. So we’re calling for increased specialist community care to ensure that people get the right support, by suitably trained professionals, to enable them to lead fulfilling lives and not end up in a crisis being placed too far from their own home, not having access to care to enable them to get better
“We’re also calling for more oversight — this is desperately needed. We want there to be a named national specialist commissioner for complex care — and we want to see a minister take ownership of this area.”
She added: “What keeps me up at night is the fact that right now there are still almost a hundred people in highly restrictive environments. The fact is that in some months there are still one hundred people admitted to environments that won’t meet their needs — more needs to be done urgently to stop people receiving the wrong care.”
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies