One in three A&E patients don't need to be there, says top NHS doctor
Professor Keith Willett said more patients could be treated by paramedics and local pharmacists
Up to a third of all patients who come to A&E wards in England do not need to be there, a leading doctor has said, in a frank admission that the NHS has not done enough to tell people where their first port of call for medical care should be.
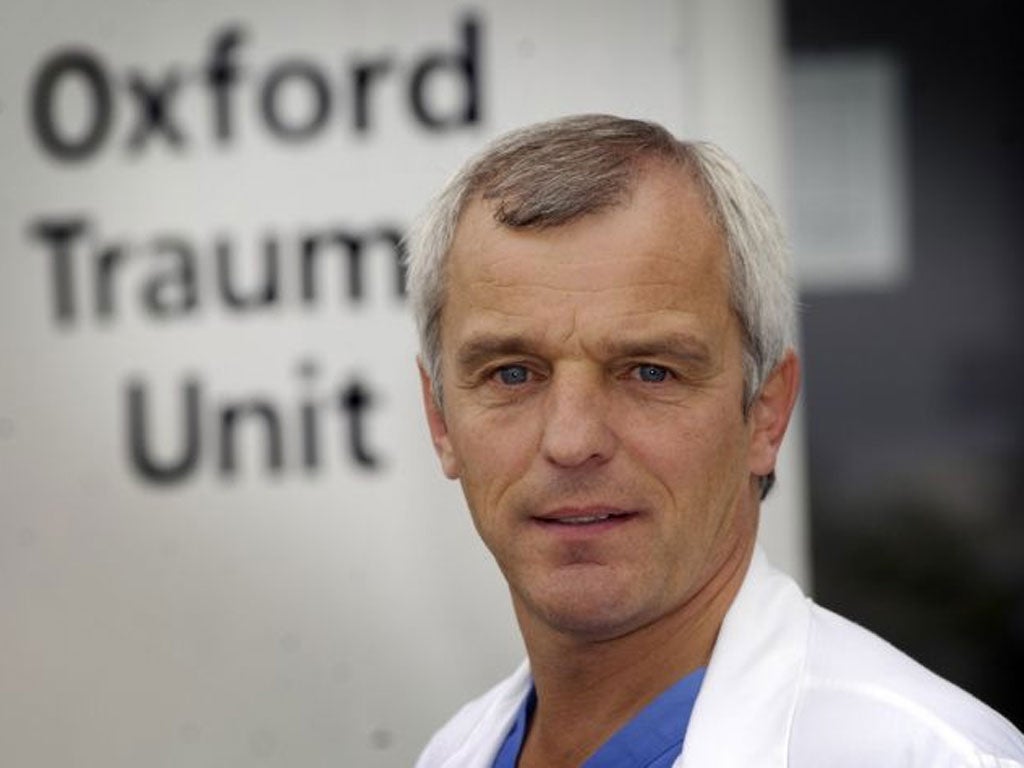
Between “15 and 30 per cent of people who turn up to A&E could have been treated in general practice,” Professor Keith Willett said. He added that more patients could be treated by paramedics, and even local pharmacists, to take the pressure off heaving A&E wards.
Professor Willett, NHS England’s director for acute episodes of care, is assisting England’s top doctor Sir Bruce Keogh in a major review of urgent and emergency care, due later in the autumn.
Too many patients, he said, did not know where to seek medical care “because the system did not obviously make itself available to them.” Patients were often frustrated at not being able to see a GP at short notice, and were frustrated by out-of-hours services, he said.
Speaking to Sky News, Professor Willett also said that patients should consider “phoning first” to find out where they should go with their condition – advice that is likely to be met with scepticism following widespread reports of poor advice and slow responses on the new NHS 111 phone line.
Last winter saw waiting times at A&E wards hit 9-year highs, with 300,000 people waiting more than four hours for treatment. MPs have warned that the country is ill-prepared for another busy winter – the time when emergency admissions annually increase.
“We would look to the public to understand the issues and when the situation does get difficult, to take the advice that I’ve suggested about phoning first, to get to the right advice, to go to the right place, to think of using your general practitioner or indeed your pharmacist, [who] give a lot of advice for minor ailments,” Professor Willett said.
He added that reducing patient numbers at A&E was particularly urgent, because efforts to reinforce the emergency medical workforce by attracting more trainees would not produce new consultants for several years.
A landmark review of emergency care is expected to recommend that all A&E wards have a consultant available seven days a week, amid fears that a lack of senior decision-makers on wards out-of-hours and at weekends is leading to patients waiting too long to be properly assessed. The report is also expected to say that paramedics should treat more patients at home or at the roadside, rather than taking them to hospital.
The health secretary Jeremy Hunt told Sky News that GPs could also take pressure off A&Es by being more “proactive” in their care for England’s growing elderly population. While acknowledging that GPs were “busy”, Mr Hunt said they should be “checking up on people, finding out how they are, [and] heading off problems before they happen”.
But GPs have warned their profession is already in a serious crisis, with increased numbers of patients, a growing bureaucratic burden and scaled down funding.
“[GPs] are overwhelmed by the workload they are expected to deliver,” said Professor Mike Pringle, president of the Royal College of General Practitioners. “We have got to start to build general practice, not blame it, not victimise it.”
Dr Chaand Nagpaul, chair of the British Medical Association’s GP Committee said: “I find it surprising that there is any suggestion NHS 111 could be used as a vehicle to signpost patients to the right treatment. In many areas it is, on a daily basis, providing inappropriate and inadequate advice that is leading to patients being on A&E when they should not be.
Far from it being a solution we think that’s something that needs to be tackled before anything else.
The important point to make is that general practice itself has seen a rocketing increase in activity. An ageing population makes for a rapidly increasing patient population with chronic complex diseases. Our workload has reached capacity. Patients recognise it’s becoming difficult to see a GP. That’s because the demand on our time exceeds our supply.
At the moment there are over a million consultations that take place in general practice on a daily basis – this is a higher level than we’ve ever seen before.
If we are to take on this work from A&Es – which we’re happy to do – we need to be enabled. That will require an expansion in the infrastructure of general practice. We need larger premises, more GPs, more nurses, more receptionists. It’s not a simple task of simply shifting patients from A&E and into the community.”
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies