The workplace is not fit for purpose when it comes to the menopause
It might be the latest buzzword in corporate feminism, but most companies are failing menopausal women, reports Rose Stokes


Until very recently, “menopause” wasn’t a word you would hear much of, unless, of course, you were a woman “of a certain age”. Even then, it would have been used or heard only in hushed circles amongst friends, or at the GP surgery. The result is that this completely normal and natural biological stage – which almost every woman will pass through in her life – is yet another women’s health issue that is shrouded in stigma and shame. This, in turn, has fostered an environment in which women at every single stage of their hormonal lifecycle know very little about this complex and largely misunderstood process.
Medical research on related issues is far behind where it should be, when you consider that 13 million women in this country are currently aged between 50 and 64, and therefore likely to be going through changes in their bodies. It has also meant that those women experiencing the varied gamut of symptoms related to “the change” (as it is sometimes also referred to) are often misdiagnosed, leading to isolation, and in many cases, contributing to large emotional events, such as divorce, or leaving their jobs.
But things are changing. Efforts by campaigners both inside and outside of the workforce are starting to yield results. High-profile female celebrities are beginning to speak out about their experiences. Calls for more progressive government policy, led by a Labour MP, Carolyn Harris, and a Conservative MP, Rachel Maclean, are attracting attention. The Labour party has recently included provision for menopause regulations at work in its manifesto. Broader coverage of menopause in mainstream news, and documentaries such as The Truth About Menopause, by Mariella Frostrup, which aired on the BBC at the end of 2018, are delivering the issue into living rooms across the country. And, indeed, menopause has become the newest focus of diversity and inclusion efforts in the corporate world – a shift that has seen companies such as Channel 4 queueing up to show off their progressive internal policies.
Medical research is bringing new treatments and surgeries to the fore as well. One particularly controversial surgical procedure that costs £10k involves cryogenically freezing ovarian tissue of women who are pre-menopausal. The tissue is then replaced when the woman is approaching menopause somewhere in the patient’s body with good blood supply, like the armpit, where it will hopefully release hormones and potentially delay the onset of menopause by as much as 20 years. The procedure hasn’t been tested rigorously yet from a safety perspective, but certainly demonstrates that science is beginning to catch up with the demand for greater understanding and treatment for women experiencing the change
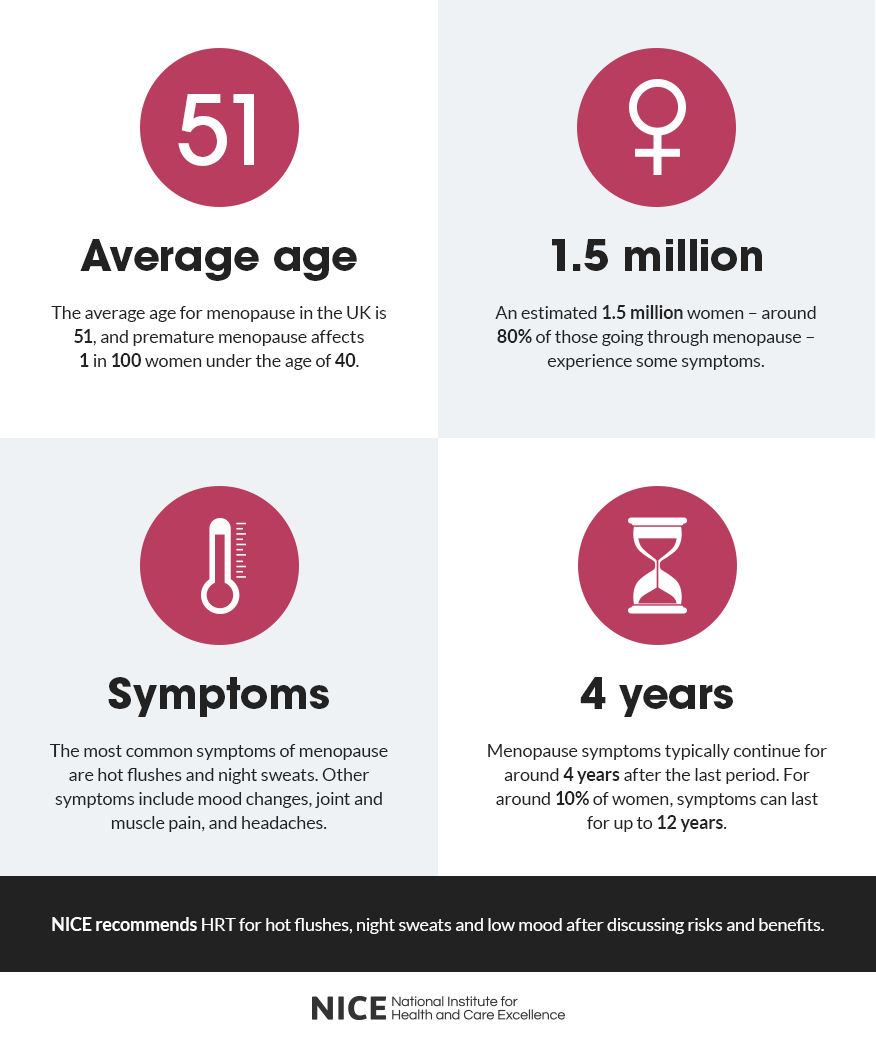
Progress is not unilaterally positive, though. Shortages of hormone-replacement therapy (HRT) since the end of 2018 – caused by supply-side issues in China that caused some manufacturers to cease production – have negatively affected up to one million women in the UK that the National Institute for Health and Care Excellence (NICE) estimates are currently receiving treatment for menopausal symptoms.

Given that HRT is the most common treatment prescribed by GPs for menopausal women, it’s not hard to see why. Misinformation is still rife, too. Links between HRT and breast cancer, which are routinely covered in the press, are overbaked, says Dr Shirin Lakhani, a doctor who specialises in womens’ post-reproductive health, and deter many women from seeking treatment. “Studies have shown that the link between HRT and breast cancer isn’t as direct as media coverage would suggest,” and “other environmental factors relating to the health of the patient, such as their weight and alcohol intake, increase their risk of developing the illness more than HRT.”
The NHS guidance on menopause says that the process usually commences between the ages of 45 and 55, giving 51 as the average age. It occurs when a woman passes out of her “reproductive phase” and usually signals a cessation of the menstrual cycle. Simply put, “it happens when your ovaries stop producing as much of the hormone oestrogen and no longer release an egg each month” says the NHS.
A woman can be classified as post-menopausal once 12 months have passed since her last period. In rare cases (1/100) this can happen in younger women aged between 30-39, sometimes as a result of other health issues, such as Down’s Syndrome or Addison’s Disease, or of treatments such as chemotherapy or radiotherapy to treat cancer.
Perimenopause refers to the stage directly before menopause occurs, when a woman’s cycle begins to change, and women can start experiencing symptoms anywhere from up to ten years beforehand, Dr Lakhani tells me. “Symptoms can be physical, mental and emotional in nature,” explains Dr Lakhani, “and there is a broad variation in the experience of different women. There’s some that will just sail through it unaffected, and some who will experience severe symptoms that require medical intervention.” However, it is thought that 3/4 women will experience some symptoms of menopause by varying degrees.
There’s some that will just sail through it unaffected, and some who will experience severe symptoms that require medical intervention
The most common symptom people think of when they hear the word “menopause” is hot flushes. This term is used to describe a sudden onset of feeling hot that radiates from nowhere in particular but spreads throughout the body, resulting in excessive sweat and feelings of stress and self-consciousness for some women. But there are many other symptoms too, Dr Lakhani explains.
“Women have oestrogen receptors all over their body, but specifically in their bones, their brain and their heart.” And given that “a woman’s oestrogen levels after menopause see an extreme drop-off equivalent to falling off a cliff,” this can have a drastic impact on patients. It also explains the wide variation in symptoms, some of which include, extreme shifts in mood, difficulty sleeping, low libido, night sweats and vaginal dryness.
A lack of oestrogen can also cause issues with bone density, leading to osteoporosis in extreme cases. “Many patients will tell me they feel completely different before and after menopause,” Dr Lakhani says. In these cases, HRT can be a life-saver for many women. “I had a high-flying patient once who refused a promotion at work on the basis that she didn’t feel that she could cope because she was experiencing such dramatic symptoms. After HRT, she feels like a completely different person.”

According to the British Menopause Society (BMS), which set out its Vision for Menopause Care in the UK in 2017, cuts to NHS budgets are “creating a climate of uncertainty surrounding menopause service provision,” despite the fact that “the effects of menopause on quality of life and later health in an ageing population are becoming increasingly apparent.” And though the launch of the NICE guideline on menopause in 2015 was a monumental moment for women’s health in the UK, “more needs to be done,’’ says Dr Lakhani.
Part of the problem, it seems, is that the majority of GPs receive only rudimentary training in identifying menopause, and therefore women are often misdiagnosed with mental health issues. People like Lauren Chiren, a menopause, women’s health and wellbeing coach, are campaigning to change this. Such efforts have yielded positive results in other areas: as of July 2019, menopause will now form part of the curriculum in UK schools, alongside pregnancy and menstruation, owing to a campaign led by Diane Danzebrink, a menopause campaigner, and MP Rachel Maclean.
According to the Chartered Institute of Personnel and Development (CIPD, an HR industry body), women over 50 are the fastest-growing segment of the UK’s workforce. Scientific and medical progress, alongside economic development over the past century mean that we are all living longer. The life-expectancy in the UK has broadly been increasing (aside from a recent small decline), and retirement ages dictated by access to state pensions suggest that we’ll all be working a lot longer than our ancestors. These demographic shifts have also been matched by a steady increase in labour participation for women over the past 50 years, with 15.3m women currently active in the workforce, according to government data. And as retirement ages have increased, so too has the likelihood of women experiencing menopausal symptoms at work.
So is it any wonder, then, in this context, that the world of work – where we all spend the majority of our time – is increasingly picking up the slack for menopausal women?
The workplace as we know it today began with the creation of dedicated “office spaces” by big companies, such as the East India Company, in the late 1700s. The post-industrial revolution period saw a rise in such office spaces, as industries such as retail, banking, transport and communications (in their early forms) took off. Since those days, the workplace has changed substantially, particularly in terms of its demographic, precipitated by the invention of human resources related functions in office spaces, in the form of “welfare managers” at the beginning of the 1900s. The CIPD, which is one of the oldest known professional HR institutions, was founded in 1914, in response to welfare concerns over women working in factories.
Although much has changed since then, regarding the social, professional and cultural position of women and other marginalised groups, workplaces have increasingly come under fire for outdated policies that don’t reflect these changes, or protect employees. It’s a shift that has seen huge global brands such as Google – whose early motto was ironically “don’t be evil” – in the firing line in recent years for the dubious treatment of women working in their organisation.
The morality of companies has also become a much more closely studied aspect of business, driving demand both in terms of sales and recruitment; put plainly, people care about who they work for, and who they buy products from. It is a trend that has, in many ways, been amplified by social media, which allows individuals to air concerns relating to the treatment of staff at work to a global audience at the touch of a button. A cursory search on Twitter for the MeToo hashtag reveals thousands upon thousands of awful experiences faced by people – particularly women and particularly at work – some of whom are willing to name and shame.

Companies are learning. An entire diversity and inclusion (D&I) industry dedicated to educating companies and staff on how to do better has risen to prominence. Many industries, particularly corporate banks, have brought in their own heads of D&I to prevent future scandals, and gesture towards the existence of a “company conscience” that takes staff wellbeing into consideration. These are all positive moves, and have led to many improvements in the workplace, as well as greater – although far from equal – representation of women, and more LGBTQ+, BAME and physically or mentally disabled people at almost every layer of business. In many ways, then, creating a “menopause-friendly workplace” is just another – albeit late – example of businesses pivoting towards another D&I metric.
And many campaigns are having real success in raising awareness in the workplace, picking up the baton where education, policy and healthcare have failed. For many women, who may have otherwise considered quitting their jobs, these policies have been a welcome step towards equality. For Lauren Chiren, who decided to leave her high-powered job convinced she had early onset dementia rather than early menopause (as it was later discovered), this is to be celebrated. “I struggled with concentration and my short-term memory, which eventually led to a situation whereby I felt I was being pushed out of the inner circle,” she says.
I struggled with concentration and my short-term memory, which eventually led to a situation whereby I felt I was being pushed out of the inner circle
Since leaving her finance job, she’s retrained as a health coach and now helps businesses and individuals think about how they cope with menopause. “It’s not just a woman’s issue,” she tells me, “it affects everyone: friends, colleagues, partners, children, doctors – we all have to take responsibility. If you know a woman, love a woman or work with a woman, this affects you too.”
When it comes to big businesses that are doing positive things with regards to menopause, she says it’s been really encouraging. “I don’t think anyone has the roadmap to get to where we need to be, but to see movement in the right direction is extremely positive.” This is a sentiment echoed by Deborah Garlick, director of Henpicked: Menopause in the Workplace, who works with major brands to train them in how best to deal with this issue in the workplace. “Raising awareness is crucial,” she says, “so individuals can start dealing in facts, rather than myths.”
But is this just another example of why the workplace, in its current state, is no longer fit for purpose? “As women and other marginalised groups become more equal in the workplace, we’re forcing a changing dynamic that means the way we view work just doesn’t fit,” explains Chiren. “Women, especially, are constantly going through cycles, be that menstruation, pregnancy, childbirth, miscarriage, termination or menopause, and all of these carry hormonal and emotional implications, alongside a wide range of symptoms,” says Dr Lakhani. “Forcing them to work within a rigid structure of 9-5, Monday-Friday and chained to a desk just doesn’t make sense,” she continues.
Forcing them to work within a rigid structure of 9-5, Monday-Friday and chained to a desk just doesn’t make sense
And the costs are high. “For every woman you lose on a £26k salary,” Chiren says, “it costs £37k to replace her. And that doesn’t even account for all the further stress caused to other staff, who may then feel overwhelmed by taking on a bigger workload and decide to leave.” She goes onto say that there is use in D&I metrics. “In business, what gets measured gets done.”

But it’s hard to understand why we keep adapting an outdated and rigid idea of “work” to accommodate changing needs in a piecemeal fashion rather than creating a new one that better represents the demands of people in the 21st century. The #FlexAppeal campaign launched by Anna Whitehouse is one of many looking for change. “I started Flex Appeal to campaign for flexible working for everyone,” she tells me. “It’s not just for mothers or fathers who want to see more of their babies, but for anyone who needs even just the smallest level of flexibility in their day-to-day lives. It’s for people with responsibilities beyond their control.
“People of any age who want to get off the 9-5 hamster wheel, people who need to work the odd day from home, people living with disabilities or anxiety, people with medical conditions, people with caring responsibilities, and people who simply want to live.” As she explains, “it’s pushing for someone to be judged on their ability to produce good work, not how long they can sit at their desk for.” Ultimately, Whitehouse says, “it’s about putting humans above business, but for business benefit.”
According to Rachel Suff, a senior adviser at the CIPD who worked on the organisations recent guidance on managing the menopause at work, we need to move towards a more “people-centric model of working”. Based on their research, almost 30 per cent of women had taken time off work because of menopausal symptoms, only a quarter of whom felt able to tell their boss about what they were experiencing. “Just implementing a policy isn’t going to solve anything,” she says, “it has to be brought to life by the company if it is going to bring about a wider cultural change.” When it comes to menopause, Suff explains: “Companies should be dealing with it as a fluctuating health condition,” rather than starting from scratch when it comes to internal policymaking. “At the end of the day, it’s about compassion. It’s about people,” she says, “companies need to put staff wellbeing at the centre of their strategy planning.”
We are still far from reaching equality for women in the workplace, but any progress in supporting menopausal women is to be applauded. However, these policies will only work if they’re followed by extensive and rigorous efforts to educate the workforce, particularly managers, on how best to implement them. Injecting more compassion into business infrastructure and strategy would help, too. And thinking long term about the benefits of a healthy and happy workforce on the bottom line is crucial.
Moves towards rebranding “human resources” functions into ones relating to “people” in many companies are a step in the right direction. After all, aren’t we all “people” rather than “resources” anyway?
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks