Mental health patients share their experiences to call for an end to stigma
As David Cameron pledges to increase mental health spending, those with mental illnesses share their stories
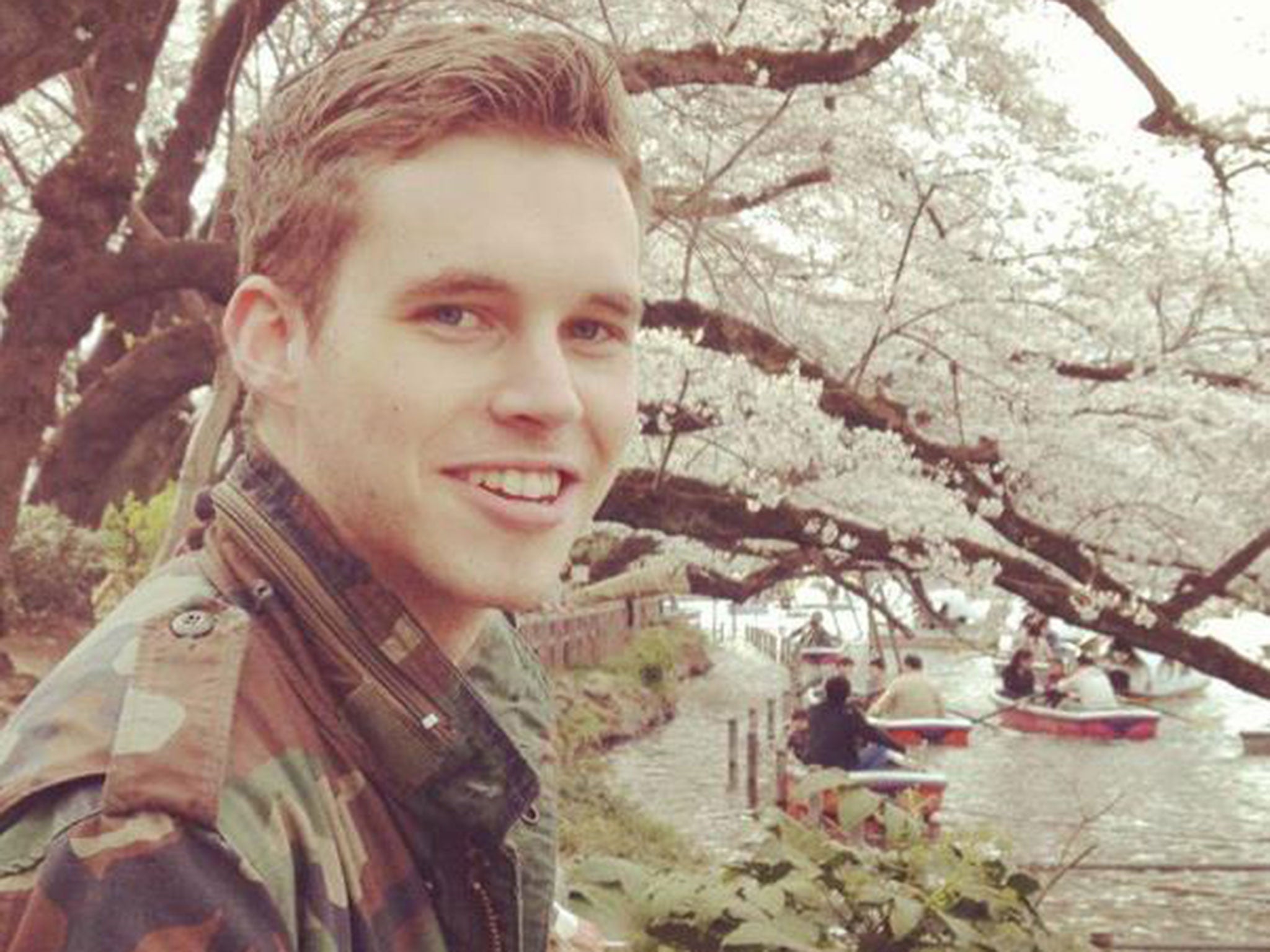
Louis Collenette, 24, was diagnosed with obsessive compulsive disorder (OCD) eight years ago. From a young age he felt he had to repeat certain tasks to prevent disastrous consequences. Four was his safe number. If he did something six times, he felt he was putting his family in danger.
When he was 12, Louis’ anxiety intensified. He vividly remembers the incident which triggered his deepest fear. He was on the tube, when he was overcome by a desperate urge for the toilet. With no toilet nearby, his brothers suggested he relieve himself in a plastic bottle on the empty tube. Terrified of wetting himself, he did. As the train drew into Ravenscourt Park station and people stared at him in disgust.
Louis was determined he would never be humiliated like this again. He became obsessed with going to the toilet. His fear of wetting himself in public took over his life. Avoidance became his coping mechanism. He skipped school and missed social events. He felt he couldn’t share what he was thinking with anyone.
“I was incredibly embarrassed about my worries. Shame stopped me from telling people I had OCD,” he says.
After years of lies and secrecy, Louis decided to share his story of living with OCD with all of his Facebook friends.
"I went from never having told anyone the whole story except my psychiatrist, to telling everyone I knew in one go. It was easier to share it in a Facebook post, than to explain it in person.”
Stigma around mental illness prevents many people from speaking out. Time to Change, an anti-stigma campaign launched in 2007 by the charities Mind and Rethink Mental Illness, conducted a survey in January of 7,171 people who have experienced mental health problems. 86 per cent says that they have faced stigma and discrimination as a result of their condition, with 64 per cent reporting that it came from friends, and a further 57 per cent from family members.
Kate Nightingale, a campaign spokesperson, says: “Our latest survey shows that nearly two thirds of people with mental health problems are left feeling isolated (64 per cent), worthless (61 per cent) and ashamed (60 per cent) because of the stigma and discrimination they have faced. Often people with mental health problems state that the stigma is worse than the illness itself.”
David Cameron promised in mid-February to help more than a million extra people and invest £1bn annually in mental health services by 2020/21.
Paul Farmer, chief executive of Mind, described the five-year strategy as “a once-in-a-generation opportunity to transform services and support for people with mental health problems.”
Rebecca Bird, 25, saw the crippling effect of stigma first hand when her mother Tracey Bird was admitted to a mental health unit.
“She didn’t want anyone to know she had anxiety. It was a massive embarrassment to her,” says Rachel.
Her mother was released from the unit because there weren’t enough beds. She killed herself a few weeks later.

After her mother’s death, Rebecca became reluctant to leave the house and started having panic attacks. The doctor immediately diagnosed her with anxiety.
She is incredibly open about her illness, and finds it worrying that mental illness is such a taboo.
"I’m determined not to let my condition ruin me like it did my mum.
"It’s fine to say you’re coming into work late because you have a blood test, but nobody ever says they’re coming in later because of counselling."
Many people who reveal their mental health problems to others are met with a negative reaction. The Time to Change survey found that 48 per cent of people stopped looking for work or returning to work because of people’s reactions when they disclosed their condition.
Nick Burnley, 31, felt stigmatised by the health care assistants who says borderline personality disorder (BPD) wasn’t a legitimate reason for him being in hospital.
"They told me I was taking up a hospital bed,” he says, adding that he received little support from his parents. “They backed away and said they couldn’t handle me when I was ill.”
However, he is keen to emphasise that others have been incredibly supportive.
“I work as a personal trainer and my colleagues have been brilliant. Out of my last 50 clients, only one or two were apprehensive.”
Louis has found the reaction to his “coming-out blog” overwhelming.
“I was convinced that revealing the truth was reprehensible. I never thought about the fact that everyone has got something they’re insecure about.”
He has since been contacted by a lot of people saying they can relate to his experience.
"One of the rugby lads from school got in touch. I’ve always been insecure about not being a manly guy and I was very embarrassed at the thought of him reading my piece.
"He’d been suffering from depression and panic attacks and wrote to me: ‘thanks for encouraging me today when I wanted to curl into a ball and pretend I was fine.’ There’s a misconception that if you’re a tough guy, mental illness is a weakness.”
Greater awareness and an honest, open dialogue are needed to break the vicious cycle of stigma around mental illness, campaigners urge.
"We need to replace silence and stigma with talking, greater understanding and support. You don’t have to be an expert to talk about mental health. A few small words can make a big difference," says Ms Nightingale.
A lack of understanding lies at the heart of the problem, Nick believes.
“They’re scared because they struggle to rationalise my condition,” he says. When asked why he thinks people with mental health problems are so hesitant to come forward, he quotes a line from the film Man of Steel: “My father believed that if the world found out who I really was, they’d reject me…out of fear.”
Investment in mental health services is urgent, Rebecca says. “At the moment the waiting list for counselling is 6-8 weeks. In the meantime your mind is just getting worse and worse.”
The report published by the NHS taskforce said that funding will help 600,000 more people access counselling services. One of the main recommendations was that £1.4bn should be invested in mental health care for children. Louis believes it is essential to raise awareness about mental illness among young people.
“I had no idea I had a condition which could be diagnosed and treated,” he says.
“I just lived with my problem in silence. I would focus all my energy on getting out of going to school. Every day I would think about letting a car run over my foot. No child should seriously have to consider that as an option.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks