Coronavirus: Global experts tell MPs how they avoided UK’s care home crisis
Zero deaths reported at care homes in Hong Kong or South Korea, compared to around 12,500 in UK
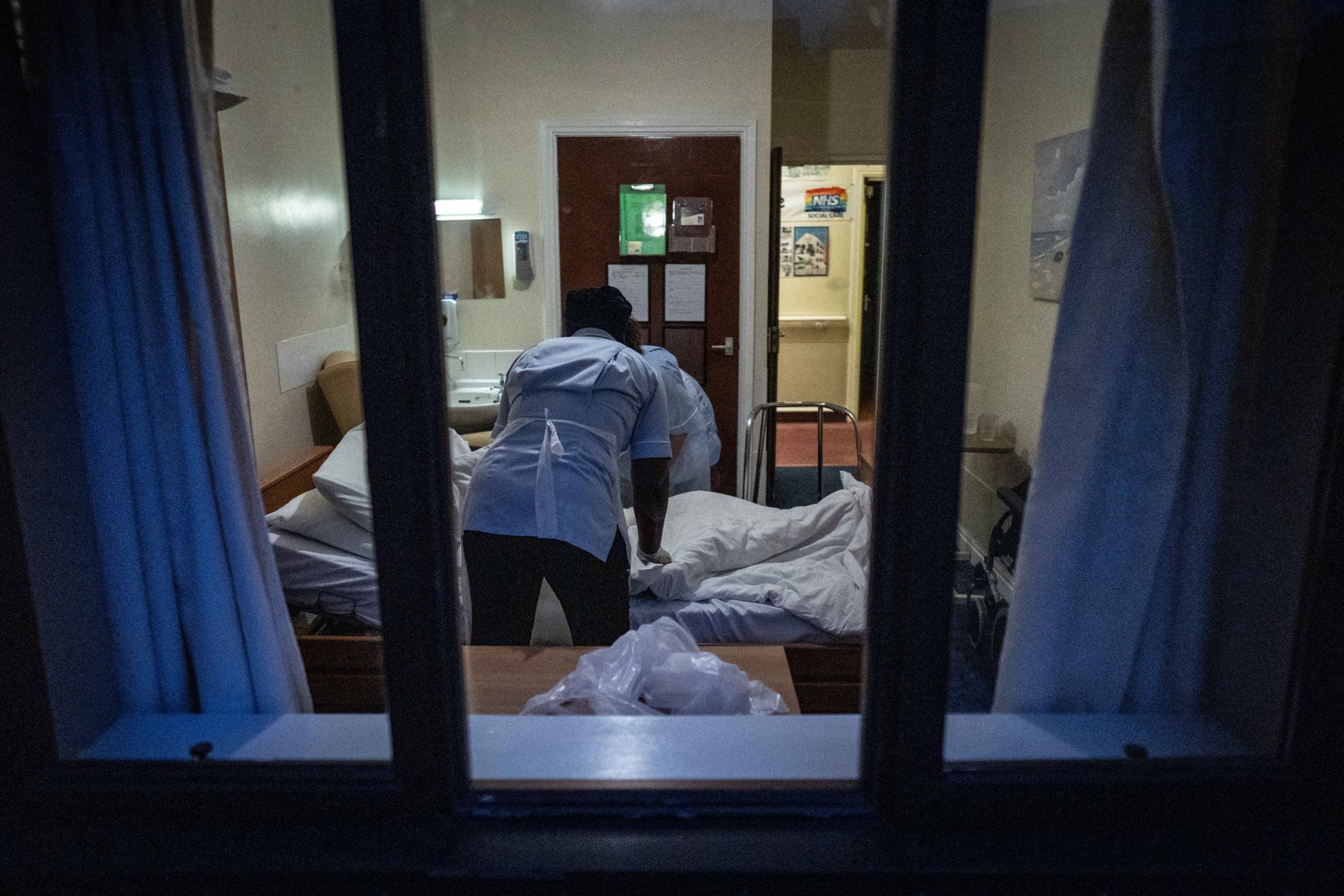
MPs have been told how countries such as South Korea and Hong Kong acted swiftly to prevent care home deaths from coronavirus as UK experts warned nursing homes were still facing testing delays, a shortage of kit and a lack of funding.
Members of the Commons health and social care committee were told there had been no deaths in care homes in South Korea or Hong Kong while in Germany the number of deaths has been limited to 3,000 compared with more than 12,500 in the UK.
Experts said this was in large part due to each country reacting quickly to the emergence of the virus and taking tougher steps sooner to isolate cases and protect care homes from becoming infected.
Adelina Comas-Herrera, from the London School of Economics, told MPs: “in South Korea, there hasn't been a single death of a care home resident in a care home.
“That is because anybody with suspected Covid was immediately isolated and if they tested positive were removed into quarantine centres, or hospitals. So not a single person has died with Covid in a South Korean care home.
"That's just an example of how quickly they acted to make sure that there wasn't any possibility of transmission within the care home.
"Singapore has adopted similar measures. They have had some infections, but they've acted really quickly to make sure that it didn't spread within the care homes."
Professor Terry Lum, head of social work and social administration at Hong Kong University, said there had not been a single care home death in Hong Kong.
He said “the first and most important” step to protecting care homes was “stopping transmission from hospital.”
Health committee chair Jeremy Hunt MP said Hong Kong’s success was an “extraordinary position” given the country “was right next door to China.”
Prof Lum added: “Efforts to control the virus started in January before a single case had been reported with people using face masks.
By late January he said 70 per cent of the general population were wearing face masks and by mid-February this was 97 per cent. Nursing home staff were wearing masks from January and stopped visits from outsiders in February, with many homes having a three-month store of protective equipment.
He said people who tested positive were isolated for three months adding: “At the same time we isolate all the close-contact people into separate isolation centres, quarantine centres, for 14 days for observation, and they did a test regularly within the 14 days to make sure they don't have the virus.”
Isabell Halletz, chief executive of the German employers' association for care homes, told MPs full protective equipment was being worn in German care homes by the end of March.
She said patients coming from hospitals had to have a negative test result and be quarantined for 14 days in a separate part of the care home.
Contrasting these examples with the UK, MPs were told there were still serious issues facing UK care homes.
Martin Green, chief executive of Care England, said pandemic planning by the government had failed to properly consider the risks for the social care sector.
He told the committee: “Our focus at the start of this pandemic was clearly the NHS and there was not a recognition in either the planning process that happened in 2016 or indeed in this current pandemic at the very start of it that the most vulnerable people were in care homes.”
Mr Green pointed to examples in Germany, Hong Kong and Singapore, saying: “Clearly when you do focus on that really central area of care homes because there are so many people in the high risk group, you can really retard the development of this virus.”
James Bullion, president of the Association of Directors of Social Services, also told the committee “we still don’t have an effective supply chain” for protective equipment to keep staff safe from infection.
He added that funding for local councils was only a quarter of what was needed to deliver care.
He said he did not think the £3.2bn provided by government “has been enough” but added “there was “firm evidence” that councils were paying money to providers, either in advance or on account.”
Speaking in the House of Commons, health secretary Matt Hancock insisted the government had created a “protective ring” around homes and had invested billions more in supporting the sector.
He said the government would look to change regulations to require more data from every care provider, and conceded that: “partial data has bedevilled the management of social care for many years.”
He added: “We need to have a more coordinated policy between health and social care, and these social care reforms, which are long overdue and have not been put in place by governments of all colours, absolutely must be.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks