Jeremy Hunt’s seven day working targets ‘not linked’ to fewer weekend deaths, says study
Chasing soon-to-be mandatory standards could "divert care" from high risk patients, authors warn
NHS standards intended to ensure senior clinicians and staff responsible for urgent tests are available at weekends have no link to reduced death rates, a study has found.
Researchers evaluated 123 NHS trusts on the seven-day working standards but found no link between performance and differences in outcomes of patients admitted at the weekend or mid-week – the so-called weekend effect.
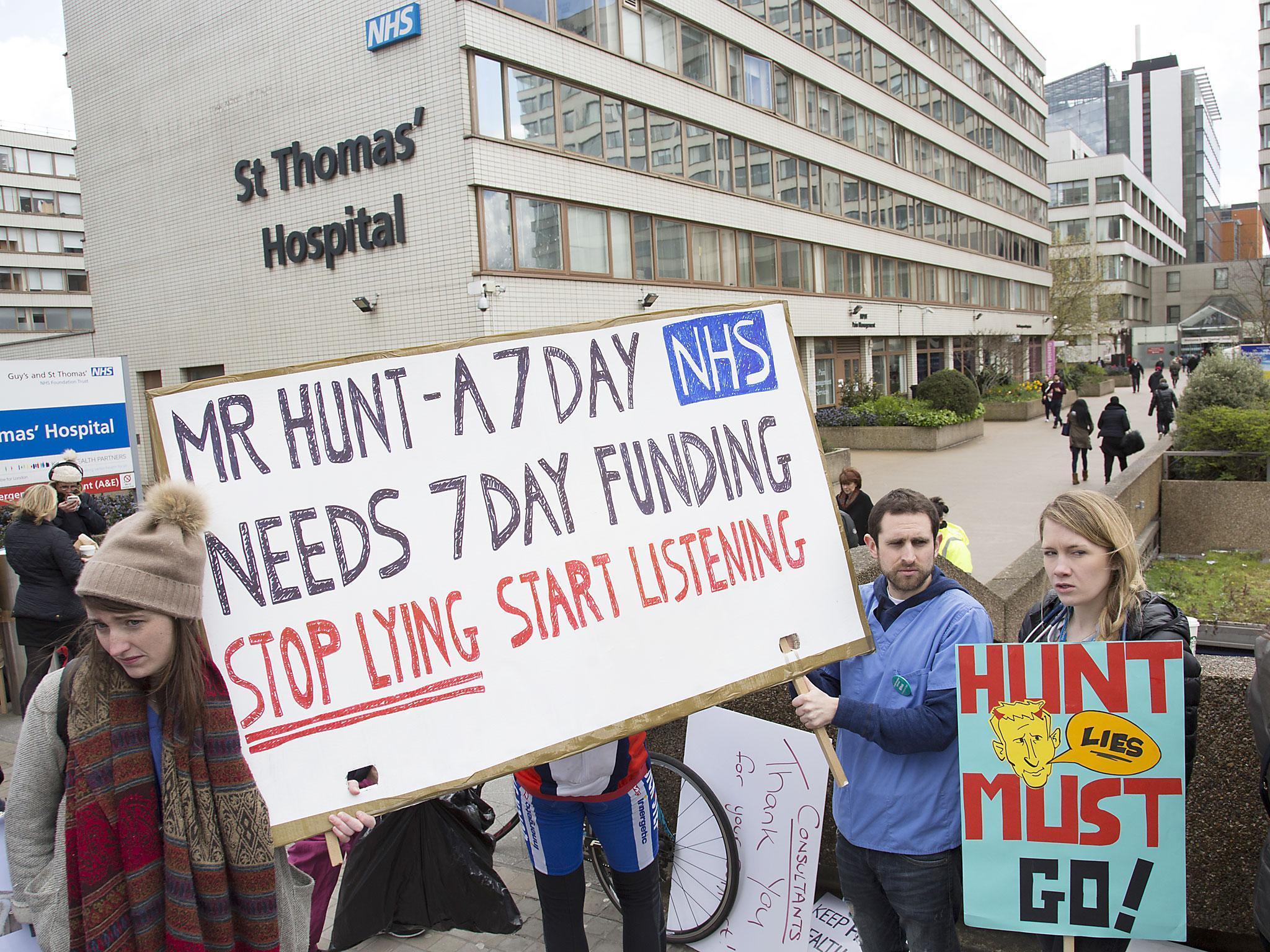
The findings cast more doubt over the evidence base used by Health Secretary Jeremy Hunt to force through a "seven-day working" contract that led to the first all-out doctors strike in NHS history.
And the study concludes that, with NHS resources being squeezed, chasing targets may “divert care away” from the most at-risk patients – though it is unlikely to cause “direct harm”.
Mr Hunt claimed on the BBC Today programme in 2015 that a shortage of weekend staffing was responsible for “6,000 avoidable deaths” a year.
Despite the author of the study he cited saying this was “inaccurate”, this premise led to the introduction of seven-day working contracts, beginning with junior doctors. It also saw “priority clinical standards for seven day services” introduced by the Government in 2015, with all NHS trusts required to be compliant by 2020. These include a requirement that emergency admissions are reviewed by a consultant within 14 hours, and that there must be seven-day access to X-rays, MRI scans and lab tests.
But other studies have demonstrated that patients who are admitted at weekends tend to be sicker already, and this could account for some of the differences in mortality.
The latest study, by researchers from the University of Manchester and published in Emergency Medicine Journal, found significant variations in trusts' performance against the seven-day standards.
Trusts were assessed before and after the standards were announced, over three years from April 2013 to March 2016.
On average, trusts met the standards for patients to have seven-day access to investigations or surgery on eight of the nine treatments specified.
Around half (54 per cent) of the recommended medical scans and tests, were available at weekends, and the average trust met the standard for a review by a consultant doctor within 14 hours of admission on five out of ten (49 per cent) of recommended medical specialties.
It also evaluated how likely a patient was to die if they were admitted midweek (Tuesday to Thursday) or at the weekend (Saturday and Sunday), and found “no association” with delivery of the standards. The authors conclude: “The results add to the increasing body of evidence questioning the link between levels of service provision and weekend death rates."
“While implementation of these standards is unlikely to result in any direct harm to patients, the requirements may divert care away from the most high risk patients, limiting clinicians’ abilities to prioritise patients based on their professional judgement.”
“The lack of association between the stated aims of the seven day services policy and the clinical standards being introduced to meet these aims suggests that the four priority clinical standards should be reviewed before compliance for all NHS hospitals is mandated in 2020."
Dr Robert Harwood, chair of the British Medical Association’s consultants committee, said: “The issue of weekend mortality is a complex one. We know, for example, that more seriously ill patients tend to be admitted at weekends, so it’s a complicated picture.
“With current services stretched, it’s important that any calls for additional staffing must be met with the necessary investment, otherwise we risk stretching existing staff more thinly, which could compromise safe patient care.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks