Blood test may detect ovarian cancer up to two years earlier, study finds
‘Around half of ovarian cancer cases are picked up at a late stage, when treatment is less likely to be successful,’ says research information manager at Cancer Research UK
A blood test may detect ovarian cancer up to two years earlier, a new study has found.
Scientists developed a simple screening method involving a biomarker made up of four proteins seen together.
The study, published in the journal Nature, involved the analysis of blood samples from 80 individuals across a seven-year period.
Dr Rachel Shaw, research information manager at Cancer Research UK, said: “Around half of ovarian cancer cases are picked up at a late stage, when treatment is less likely to be successful. So developing simple tests like these that could help detect the disease sooner is essential.
“At Cancer Research UK, we’re working hard to find new ways to detect cancer early and improve the tests already available. It’s really exciting to see these encouraging results for this type of ovarian cancer.”
The NHS states ovarian cancer is one of the most common types of cancer in women – saying overall, around half of women with ovarian cancer will live for at least five years after diagnosis, and about one in three will live at least 10 years.
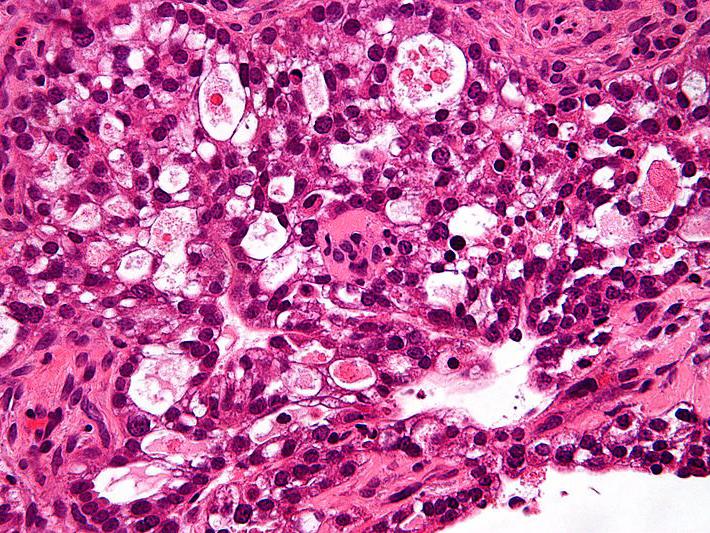
Dr Bobby Graham, the study’s lead author, said: “Firstly, we discovered that the presence of the biomarker panel will enable us to detect Epithelial Ovarian Cancer (EOC).
“We then developed a screening test to detect this biomarker panel, making this a relatively simple diagnostic test.”
Dr Graham, from the School of Biological Sciences at Queen’s University Belfast, added: “The algorithm designed will screen the blood sample and flag any abnormal levels of the proteins associated with the cancer. The screening test identifies ovarian cancer up to two years before the current tests allow.”
For women in the UK, ovarian cancer is the sixth most common cancer. In 2016, 4,227 deaths were reported as a result of EOC.
If diagnosed at stage one of EOC, there is a 90 per cent chance of five-year survival compared to 22 per cent if diagnosed at stage three or four.
Dr Graham said the results of this study are encouraging but they now want to test it in a wider sample set so they can use the data to advocate for an ovarian cancer screening programme.
Additional reporting by Press Association
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks