Scientists discover protein that helps trigger allergic asthma
Scientists have discovered a blood clotting protein they believe contributes towards allergic asthma, a finding that could help develop more targeted treatments in the future.
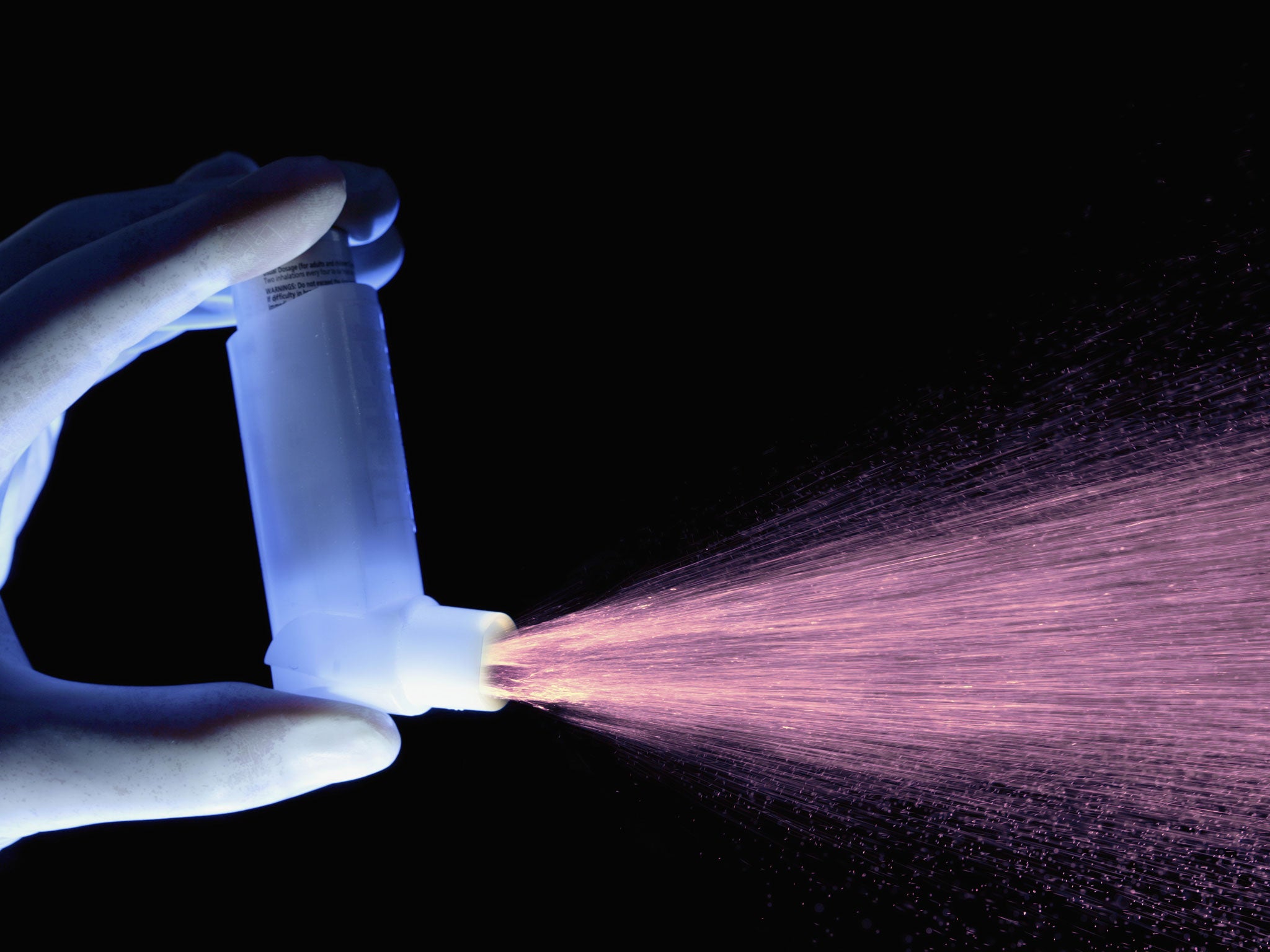
Allergic asthma is often marked by symptoms like difficulty drawing breath, wheezing and coughing, and can be trigged by different factors in the environment such as dust, mold or animals.
Co-author David Corry explained that "asthma is part of a battle that takes place as the immune system marshals its forces to fight off an invading organism-or what mimics such invaders."
This "fight" significantly affects the human airway and lungs, generating an often violent and potentially deadly reaction - asthma.
Researchers at the Baylor College of Medicine in Houston induced allergic reactions in mice by exposing the animals the proteinases found in mold.
These proteinases break down a blood-clotting protein called fibrinogen. The resulting pieces of fibrinogen bind to and activate the TLR4 pathway.
Dr. Corry found the same fibrinogen fragments that are part of the blood clotting process can cause clotting that creates a barrier to breathing and inflammation, triggering allergic asthma.
But when the team prevented this fibrinogen breakdown, the mice had a reduced reaction to mold spores.
This also occurred in mice lacking TLR4, suggesting that both proteins are part of a protective biological chain of events in some people, but not others, according to Science News.
"We suspect asthma is a protective response against fungi in many people", Dr Corry said. But in others, “it’s an aberrant response induced by extreme sensitivity to the proteinases.”
Stephanie Eisenbarth, a physician and immunologist at the Yale School of Medicine told Science News that these findings "made perfect sense".
“Fibrinogen may be a canary in a coal mine — acting as a detector of something pathogenic that may not be detected by classic mechanisms,” she said.
Dr Corry argues the findings give a further insight into the TLR4 pathway, but the specifics of allergy and immunity are still being investigated by scientists.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks