UK-first surgery removes patient’s ‘inoperable’ tumour via eye socket
Patient, a mother of three, had tumour beneath her brain
Medics have performed a UK-first operation to remove a type of head cancer deemed “inoperable” using keyhole surgery through a patient’s eye socket.
Mother-of-three Ruvimbo Kaviya had a meningioma removed from the space located beneath the brain and behind the eyes.
Many of these types of tumours would have previously been considered inoperable by doctors as they are situated in an area called the cavernous sinus.
And those which have been removed require complex surgery which involves taking off a large part of the skull and moving the brain to access the tumour – which could lead to complications like seizures.
But now surgeons from Leeds Teaching Hospitals NHS Trust managed to remove one of these tumours using keyhole surgery through Ms Kaviya’s eye socket – the first surgery of its kind in the UK.

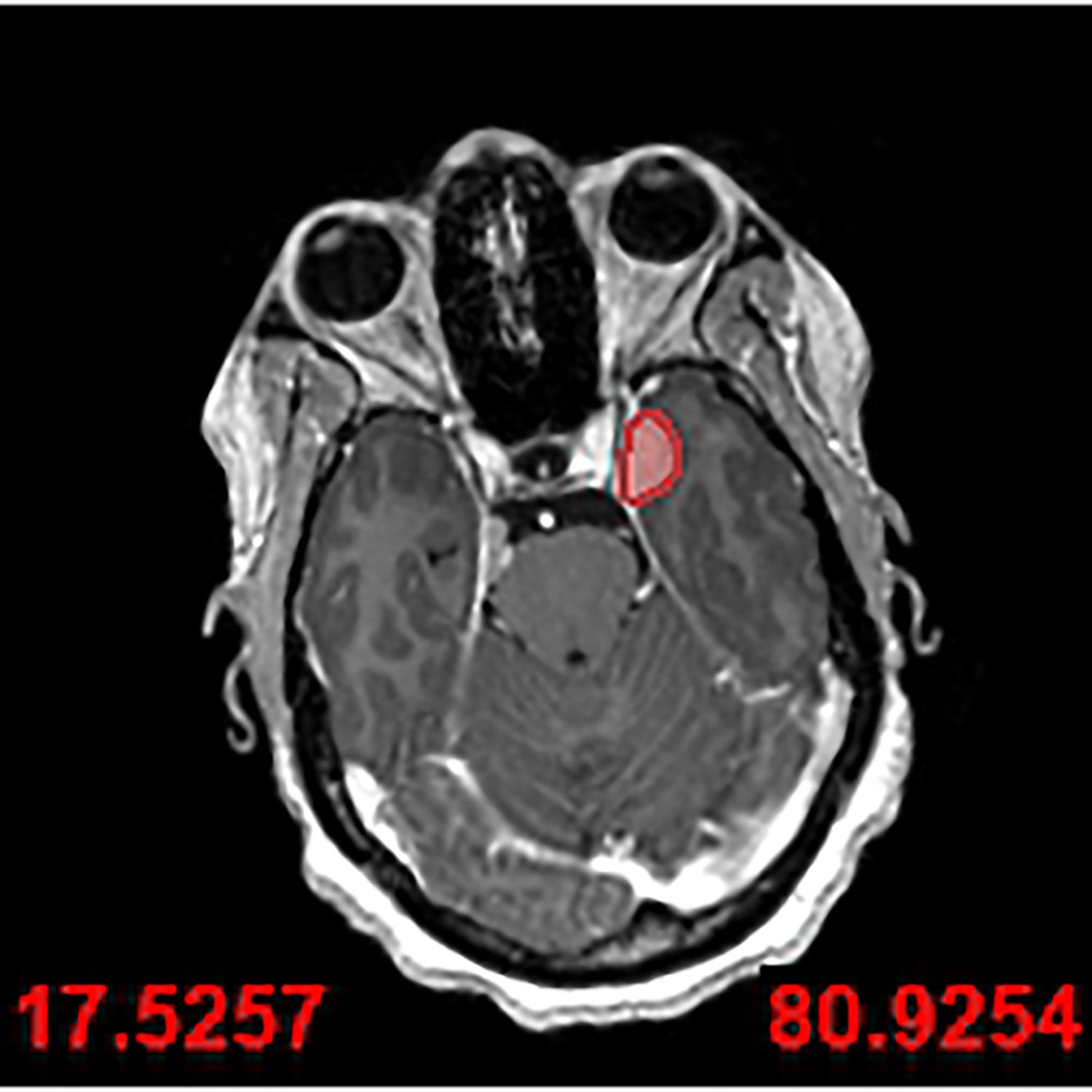
Experts at Leeds Teaching Hospitals NHS Trust practised the surgery multiple times – first using 3D models of Ms Kaviya’s head and then in a cadaver lab.
The surgery, known as an endoscopic trans-orbital approach, took just three hours and Ms Kaviya, a nurse in Leeds, was up and walking about later the same day.
“There’s been a move towards minimally invasive techniques over the last few years or so, with the advancement of technology, tools, 3D innovation, it is now possible to do the procedures with less morbidity, and that means the patients recover quicker and better,” neurosurgeon Asim Sheikh, told the PA news agency.
He said traditional methods to get to the place where the tumour was situated require “pressing on quite a lot of brain”.
“So if you press on it too much, or retract it, or try and move it apart, then it can lead to patients having seizures afterwards. Whereas this way, we’re not even sort of touching the brain,” Dr Sheikh said.
“It’s a hard-to-reach area, and this allows direct access without any compromise of pressure on the brain. So it just reaches us in areas which are once thought to be inoperable, but now are accessible,” he said.
His colleague Jiten Parmar, a maxillofacial surgeon, devised a technique where a little part of the outside wall of the eye socket was cut to allow more access for the endoscope.
“We innovated a new technique, which I think is unique to Leeds, to make the operation much easier,” Dr Parmar said.
He said that before this new keyhole technique, the area that needed to be operated on was “difficult to get to from the outside without taking off most of the skull plate” which in itself can cause some quite serious damage.
“Going through the eye socket gets into the same area and it’s a way more elegant approach. It reduces the morbidity for the patient because you disturb your blood vessels and fewer nerves,” Dr Parmar said.
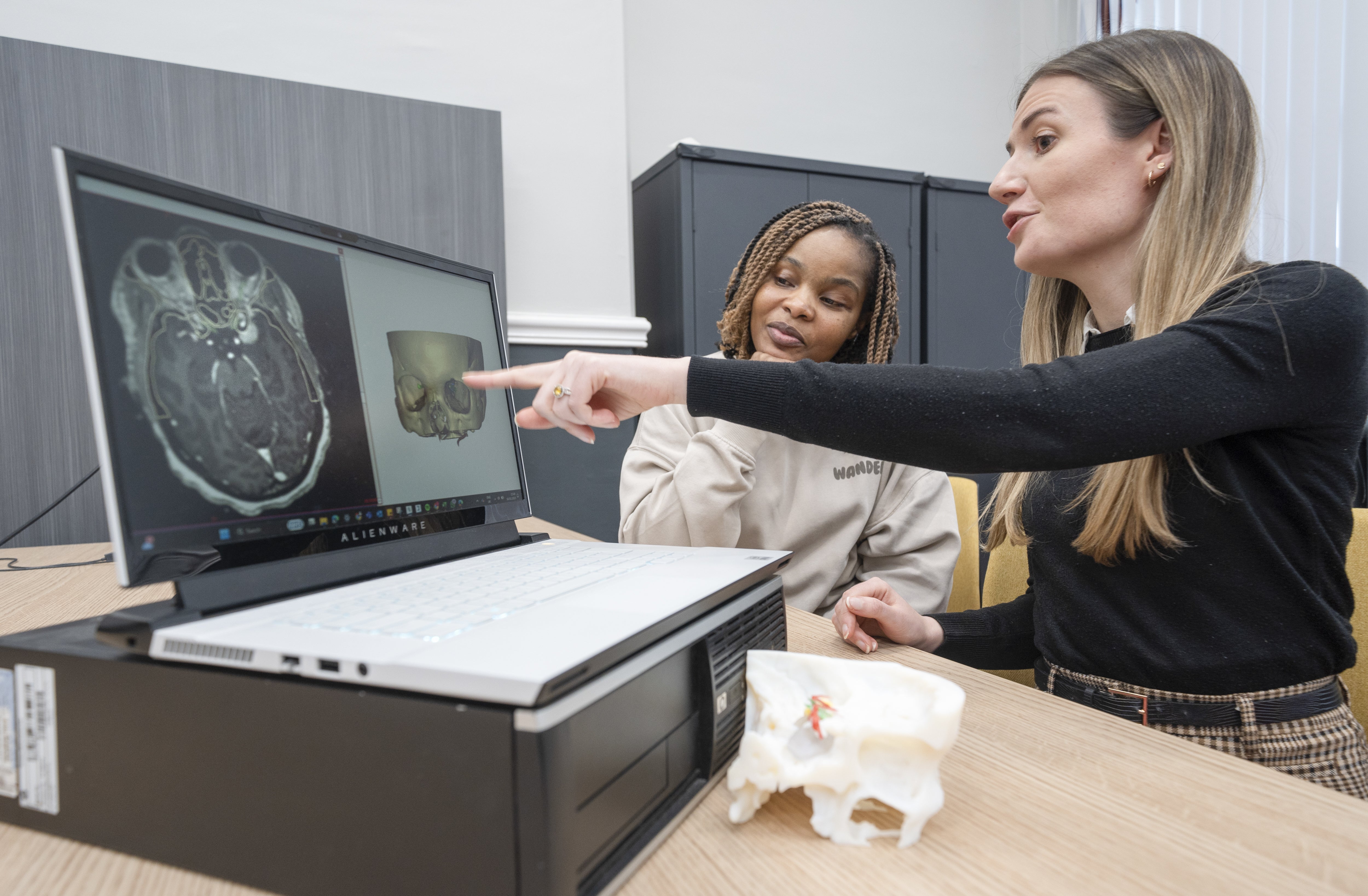
Lisa Ferrie, biomedical engineer and head of the 3D planning service at Leeds, made a 3D model of the patient’s skull so the surgical team could rehearse the operation before they did it.
“When the surgical team approached me, we used scans of Ruvimbo’s brain and skull to create a 3D replica model,” Ms Ferrie said.
“This technology enabled the team to study her anatomy in detail and prepare for the procedure with unparalleled accuracy,” she said.

James Robins, a fellow in neurosurgery, said the operation through minimally invasive techniques was still a massive surgery.
“Using the endoscope, it’s about five millimetres in diameter, we only need a very small space in order to gently displace the eye to one side to get to the back of the eye socket, removing a small, tailored amount of bone,” he said.
“And that’s where Lisa comes in. She enables us to model this patient’s skull beforehand to tell us exactly how much bone we can remove, and then we can remove the precise amount of bone, and then we can remove the tumour, usually from inside out, and just gently, down for a small operative corridor,” the neurosurgery fellow said.

Ms Kaviya said that she did not even think about being the first UK patient to undergo such a procedure because the tumour was causing such severe headaches.
“I had some headaches which felt like an electric shock on my face. I couldn’t even touch my skin on the face, I couldn’t eat, I couldn’t brush my teeth, it was really terrible,” she told PA.
She was eventually diagnosed with a meningioma in 2023 with a second one also found in October that year.
Medics at Leeds consulted experts in Spain who said she would be a good candidate for the new surgery, which was then performed in February 2024.
The 40-year-old nurse needed three months off work after the surgery but is now back caring for patients in Leeds.
“It was a really tough time, I was told I had one tumour and then told I had another, I don’t know how I managed to cope. It was very stressful and difficult,” she said.

“So when they told me that they’re going to do the surgery – they couldn’t say that it was going to be perfect and there was risk involved.
“It was the first time they were doing the procedure. I had no option to agree because the pain was just too much – I didn’t even think about it being the first time, all I needed was for it to be removed.”
Ms Kaviya, whose three children are aged eight, 12, and 13, said her family were “sceptical” about the procedure, adding: “But I just, I just told them that ‘I just have to do this – it’s either I do it or it, it keeps growing, and maybe I will die.”
“There’s a first time to everything. So you never know, this might be the best chance for me to have it’. And it was.”
On her recovery, she said: “When I had the operation I thought I was possibly going to stay in the hospital for weeks or months and I was home in days.
“I had double vision for about three months but everything else was OK.”
She said she has been left with a “really tiny” scar.
“If you don’t really look closely, you won’t be able to see,” she added.
Bookmark popover
Removed from bookmarks