I have patients with incurable brain tumours, psychosis and Parkinson's – and all of them were declared fit for work by the DWP
One patient has daily headaches, is tired all the time from chemotherapy and has horrible side effects from radiotherapy. Yet the DWP has rejected his claim
As an NHS GP, I’ve known some of my patients and their families for 10 years or more, and I can see the impact of their illness on their social, personal and working lives. I see this impact hit even harder when they are denied the benefits they need, which is a frequent scenario at my surgery.
Before I became a family doctor, I grew up with a strong work ethic. But even medical school could not prepare me for dealing with the challenges faced by my patients when it came to their financial stability. One would assume that a doctor who assesses their patient as unfit for work or in need of disability assistance would simply sign a standard form and the patient would receive their benefit entitlement. It should be that simple, but it often isn’t.
I’m immensely proud of our NHS and national benefits principles: as a society we aim to help those who are struggling with illness so that they do not have to bear the burden alone. Yet there is a lot of talk about people who “work and play the system”. From my experience of 14 years in the NHS, there are far more patients who genuinely need benefits and help than people who feign medical problems to obtain financial gains.
This is where the frustration and the outrage about the benefits system begin.
I recently received notifications from the Department for Work and Pensions that my patients have had a work capability assessment and they are deemed as fit for work.
This can be true in some instances and I embrace a culture of encouraging patients to engage in manageable employment. However, this isn’t the case for a lot of them.
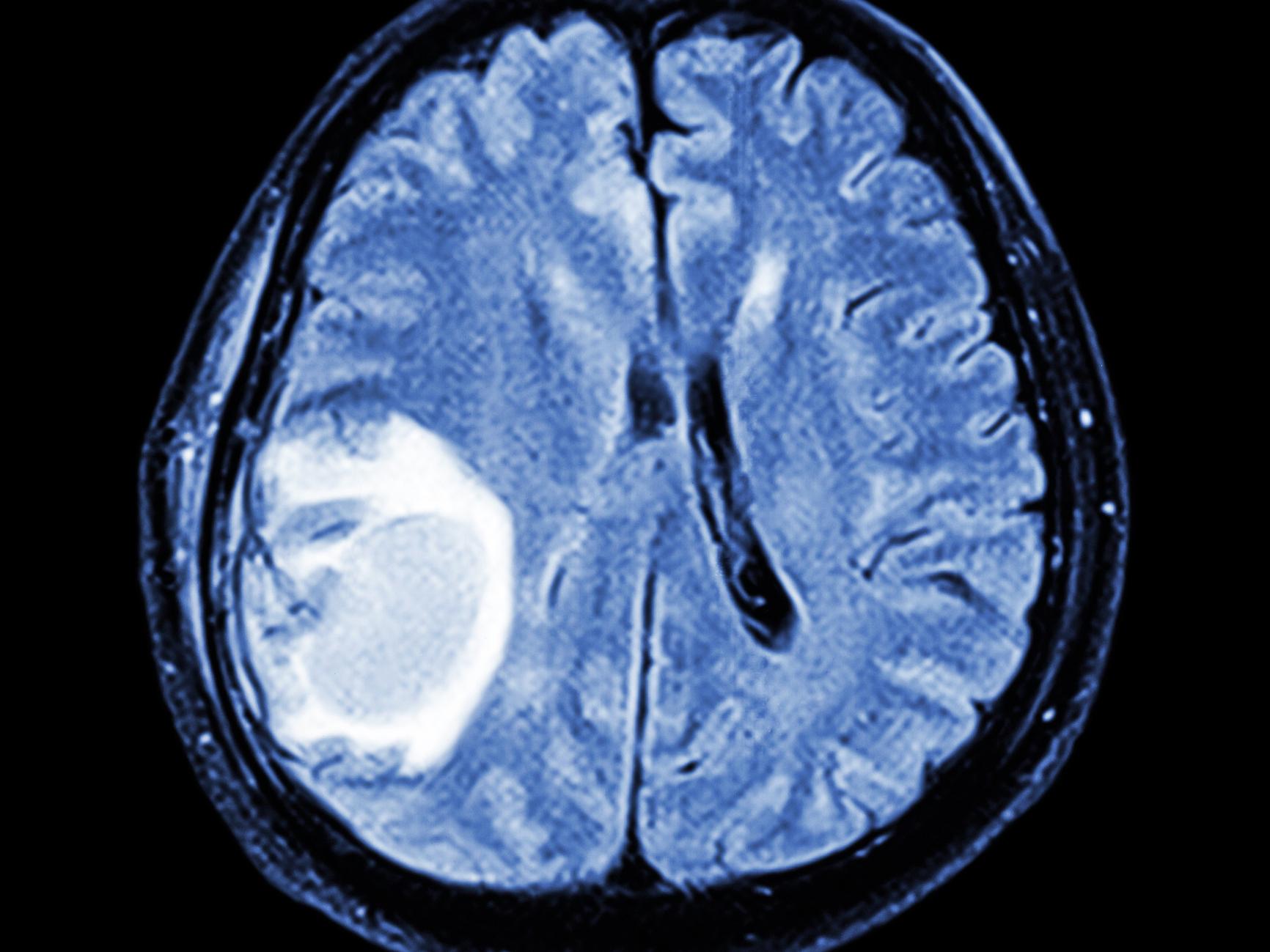
Let’s talk about my patient who has an incurable brain tumour. He has daily headaches, is tired all the time from chemotherapy and has horrible side effects from radiotherapy. He is most certainly not fit for work, yet the DWP thinks he is.
Similarly, I have a working age patient with a really unfortunate diagnosis of early onset Parkinson’s disease, which is a neurodegenerative condition. The patient has an uncontrollable tremor in both arms, shuffles when walking, sometimes cannot initiate movements and then suddenly stops (ie freezes). The patient’s spouse has to put food in their mouth as the tremor means it is difficult to handle cutlery, as well as help the patient get dressed and go to the toilet. This patient is significantly disabled by this condition, and yet the DWP says there is no entitlement to the PIP disability benefit. The patient felt humiliated by the assessment because, having worked since leaving school, they were made to feel like a “scrounger”.
There are more examples, including my psychiatric patients who cannot function in employment due to schizophrenia, paranoia and learning disabilities. They shouldn’t have to go through this stress, and, although patients can appeal, they shouldn’t have to when their diagnoses are so clear.
The recurrent theme I hear from patients who have been to such assessments is that they are short, 10-minute appointments and they do not take into account the patients’ limitations. Could my patient with Parkinson’s disease walk into the assessment room and pick up a cup? Quite possibly in that snap shot of time. But what about during the remaining 23 hours and 50 minutes of the day? The luxury of my relationship with the patient is that I have often known them for months or years. I know the struggles they face and I can see how their disease impacts on their daily activities.
At our GP surgery, we recently set up a Wellness Centre, where we have regular citizens advice helpers who can come to give relevant advice to our patients about how to access further help and appeal. Some of our patients find reading and writing difficult so they are given assistance with filling out forms and understanding correspondence. I am currently in the process of writing a letter about my patient with the astrocytoma brain tumour to appeal the decision (this will be in between my surgeries, pile of referrals and blood results, home visits and practice management tasks).
It seems that the current system is not working for those who need it, and NHS time and resources are being drained in trying to correct a problem that shouldn’t exist in the first place.
Mayjay Ali is a family doctor who specialises in dermatology, elderly care and health and wellbeing
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks