NHS’ ‘slapdash’ cost-cutting leaving thousands without vital treatment
Exclusive: NHS England cut its funding for pectus surgery in 2019


Thousands of children and adults are being forced to live with a debilitating condition after the NHS cut funding for its treatment, The Independent can reveal.
Leading surgeons have voiced their concerns that an estimated 3,000 children and adults in England living with the rare congenital condition pectus are missing out on life-changing surgery following “slapdash” cuts to the service.
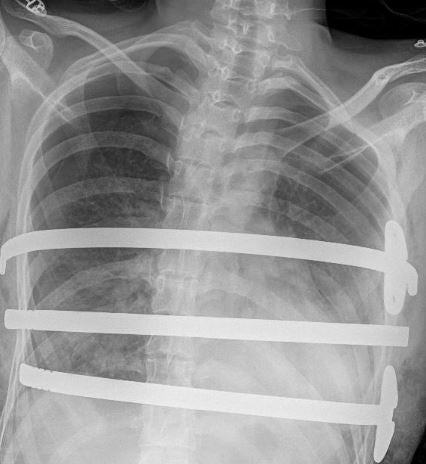
The condition involves a deviation of the chest bone – or sternum – meaning that it either grows inwards towards the spine, leaving a scooped-out appearance in the chest (pectus excavatum), or grows outwards (pectus carinatum). In the most extreme cases of pectus excavatum, heart and lung function can be affected, causing breathlessness, fainting, and even crushed heart valves.
While patients in Scotland, Wales and Northern Ireland can still undergo surgery for the condition, NHS England cut funding for this treatment in 2019, saying there was not enough evidence of the clinical benefits of the procedure, despite acknowledging the severity of some cases.
The Independent has heard stories of patients left “trapped”, having to crowdfund thousands of pounds to pay for private treatment, and being forced to travel hundreds of miles to Scotland just for advice.
Parents have also described how their children developed severe mental health problems, are missing school, and cannot walk without becoming breathless. Some are having to use wheelchairs.
Leading medics have now called for an overhaul of the panel NHS England uses to make decisions on funding specialist care.
‘Trapped in their conditions’
Dr Simon Kendall, a former president of the Society for Cardiothoracic Surgery, told The Independent that NHS England “absolutely trapped these young people in their conditions” when it decommissioned the service.

Mia-Rose Shaw-Wass, 10, has the most “severe case” of pectus excavatum ever seen, according to Dr Joel Dunning, one of the remaining specialists in the condition in the UK. She has just a one-centimetre gap between her chest bone and backbone.
Her mother, Kirsty Shaw, is having to take her hundreds of miles from Nottingham to Glasgow for consultations. Last summer, NHS England acknowledged the need to fund surgery for life-threatening cases, which Mia’s case would qualify as, but the funding has still not been confirmed.
Ms Shaw said Mia-Rose was eight when she started having fainting episodes just while walking to the shops.
“We couldn’t get her to go to school because she’d become so anxious about fainting,” she explained. “We’ve worked with the school to finally get her in, but I’m having to use a wheelchair to bring her home, because on the walk home, which is about 20 minutes, she’ll feel faint halfway there.
“She wasn’t leaving the house at all, only to go to school. She has panic attacks. She says: ‘Mummy, if I don’t have the operation and the gap gets smaller, will I die?”
‘No quality of life’
Eddie was diagnosed with pectus at the age of 13 in 2019, his mother Lizzie Cushway said. He was referred to a children’s hospital, but his mother was told there was no service and that his family would have to “prove” his suitability for an operation through an individual funding request.
Ms Cushway said a string of subsequent appointments have trigged severe obsessive compulsive disorder in Eddie, and he has been referred to children’s mental health services. She said he suffers from extreme mental and emotional distress. “He has to sit in a foetal position to manage his rib pain and scoliosis caused by the pectus. He has no quality of life.”
Lynne Evans, who launched a patient campaign group gathering stories of patients affected by pectus, has two sons who suffer from the condition.
She said: “Nearly everyone is being told treatment is not available because it is a ‘cosmetic’ condition, but it is causing severe physiological health conditions, devastating mental health conditions, their chests being crushed, and air being squeezed out of their lungs.”
Patients can still be treated using non-surgical measures, such as wearing a chest brace, but the treatment available depends on what has been funded by local NHS commissioners. After funding for surgery was cut, 25 out of 26 specialist services across England were closed to referrals.
“Patients, especially young patients, are being failed at the first hurdle, which is the GP practice. [They feel] helplessness and frustration at this utter lack of a treatment pathway. It’s ludicrous that patients with the same condition in Wales, Scotland and Northern Ireland can receive treatment, but we can’t in England,” said Ms Evans.
‘Slapdash’
Dr Dunning told The Independent he gets weekly emails from patients whom he cannot treat but who just want advice. “It is devastating. I have just reams and reams of people – totally frustrated and stuck at home – who know there’s something that can fix them that they can’t have,” he said.
Dr Dunning criticised the process NHS England used to cut the service, saying: “The whole thing has been set up in a slapdash, cut-price way.”
In November 2020, the issue was raised in parliament by Tory MP Simon Clarke, who said the NHS commissioning process had “failed”. He said it was unreasonable that treatment would never be available, irrespective of the seriousness of the symptoms.
He went on to claim that the average cost of surgery is between £7,000 and £16,000, meaning that treating even the 50 most severely affected patients each year would cost less than £1m – a “minute sum of money” in the context of the wider NHS budget, he said.
NHS England said last year it would look to fund care for the most severely affected but, six months on, no funding or policy has been finalised. Dr Dunning added that the policy would only mean that the “tip top of the iceberg” of patients would get care.
NHS funding for specialist services – how does it work?
Specialist care is funded through the national NHS budget, which is controlled by NHS England. There is a finite budget to spend each year, and so NHS England reviews annually which services it can afford to maintain within the constraints of its funding.
The national body has a team called the Clinical Priorities Advisory Group (CPAG), which decides which services NHS England should pay for.
A total of 160 specialist services are currently paid for routinely and can be accessed by patients. However, in the last five years, 65 specialist services, including those covering pectus, have been cut following a review by the CPAG. Other examples of services the NHS has decided not to pay for routinely include some robotic-assisted surgery and hyperbaric oxygen therapy.
‘Life-changing’
While patients in England can no longer access care for pectus, surgeons in Scotland have set up a service to which children can be referred, which offers them input from paediatric surgeons, physiotherapists and clinical psychologists.
Ellie Musgrave, 27, had an operation for the condition in 2018 before the service was cut.

She told The Independent that, before her surgery, she could “literally feel her bones crumbling”. “It was very, very painful. As well as that, it was like I was literally having the air pulled out of me,” she said.
When she was 21, her health had so “profoundly declined” that she couldn’t walk to university. She was “isolated” and her mental health was “shocking”, she said.
However, she said, surgery “completely transformed” her life. “Whereas before I was declared unfit to work, I [now] work full-time. Before, I was being cared for by my parents; I [now] live with my boyfriend, and I’m not being cared for, I’m active for the first time in my life,” she said.
An NHS spokesperson said: “The current decision to not routinely commission this surgery is based on advice from doctors and insufficient evidence to support its benefits.”
It said some patients experience very severe cardiac and breathing problems, and that it is creating an “urgent” policy for such cases, which will be based on new evidence being published.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks