Cancer screening has never been shown to save lives, experts claim
Researchers say false results causing deaths from needless treatments are not being taken into account
Cancer screening has never been shown to save lives, experts claim as false results causing deaths from needless treatments, along with suicides or heart attacks, are not being taken into account.
Researchers say that, whereas the harms of screening are certain, the benefits in overall mortality are unclear. The belief screening prevents early deaths is based on reductions in disease-specific mortality rather than overall mortality, which should be the benchmark against which screening is judged, they argue. Support for programmes that borders on fear-mongering has led to the public having an inflated sense of the benefits and discounted sense of the harms of screening, scientists from the Oregon Health and Science University write in a BMJ article.
The authors cite screenings of prostate and breast cancer as particular examples where further testing, overdiagnosis and overtreatment can cause more harm than good. Realisation of this in other areas has led to reversal or abandonment of a number of screening campaigns, including chest radiography screening for lung cancer and urine testing for neuroblastoma, they write.
The scientists say prostate-cancer testing yields numerous false positive results, which contribute to over one million prostate biopsies a year. These, in turn, are linked to serious harms, including admission to hospital and death as men diagnosed with prostate cancer are more likely to have a heart attack or take their own lives in the year after diagnosis.
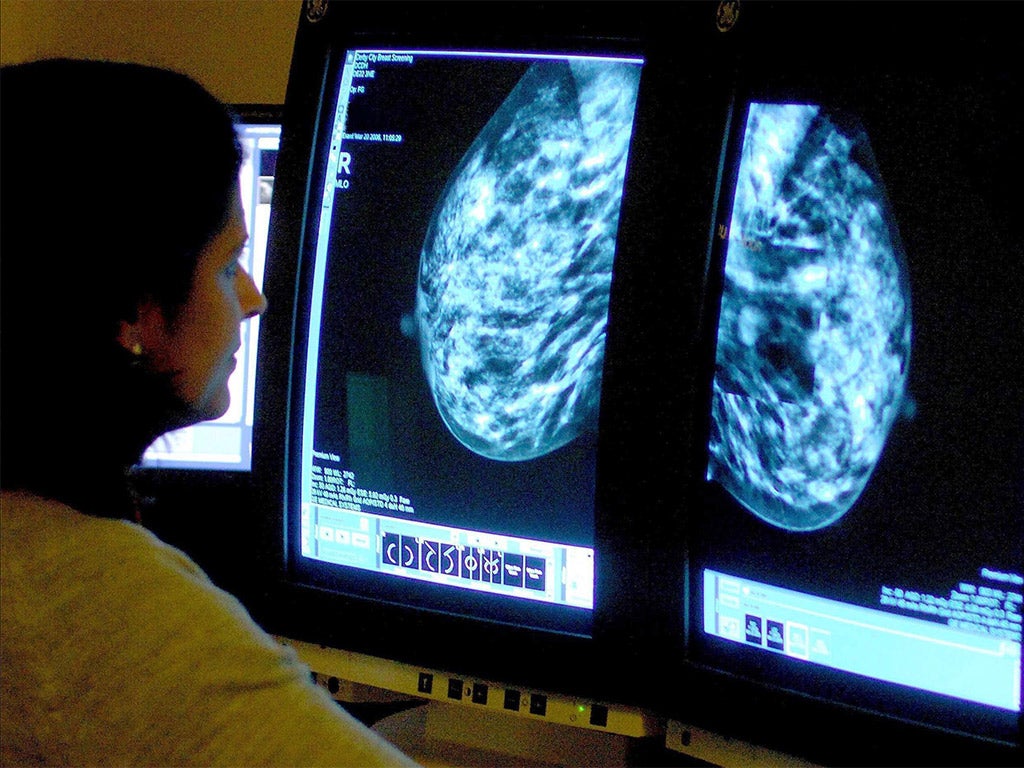
Although studies regularly show women think that breast screening lowers their risk of getting breast cancer, a recent mammography review in the United State “did not show reduced breast cancer deaths when adequately randomised trials were analysed”, the scientists write.
Cancer screening
There are three NHS Population Screening Programmes that relate to cancer. They are:
- NHS bowel cancer screening (BCSP) programme - offers screening every two years to all men and women aged 60 to 74. People eligible for screening receive an invitation letter explaining the programme, along with an information leaflet explaining the benefits and risks of screening.
- NHS breast screening (BSP) programme – offered to all women aged 50-70. Women do not always receive an invitation when they turn 50. They can expect their invitation within three years of their 50th birthday. Women cannot walk in and request breast screening unless they are over 70, when they can request screening every three years. In some areas, women aged 47 to 49 and 71 to 73 receive invitations for screening. This is part of a study looking at whether to extend the breast screening age range.
- NHS cervical screening (CSP) programme - available to women aged 25 to 64 in England. All eligible women who are registered with a GP automatically receive an invitation by mail. Women aged 25 to 49 receive invitations every three years. Women aged 50 to 64 receive invitations every five years.
Consideration of harms also becomes more important in the absence of clear overall mortality benefit, they add. To find out whether screening saves lives, they say investing in large trials that can determine overall mortality is “worth the expense compared with the continued cost of supporting widespread screening campaigns without knowing whether they truly benefit society”.
The team calls for “higher standards of evidence”.
However, the scientists said political will, financial resources, and public perception are “common hurdles” in building support for measures likely to be costly and take time and effort. They conclude: “We encourage healthcare providers to be frank about the limitations of screening – the harms of screening are certain, but the benefits in overall mortality are not. Declining screening may be a reasonable and prudent choice for many people.”
An accompanying BMJ editorial calls for more “transparent information” on cancer screening.
Samia al-Qadhi, chief executive at Breast Cancer Care, said the study added to the “mountain of conflicting evidence” on screening.
She added: “This ongoing confusion about the benefits and risks of screening means that women are unsure about whether to attend. It’s one of the reasons why the number of women going is declining.”
Dr Anne Mackie, director of screening at Public Health England, said: “NHS cancer screening and follow-up treatment does prevent or can at least delay some people dying from cancer.”
Subscribe to Independent Premium to bookmark this article
Want to bookmark your favourite articles and stories to read or reference later? Start your Independent Premium subscription today.

Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies