This super bug is spreading across half the US
The fungus poses a greater risk for vulnerable populations in nursing homes and hospitals
A deadly fungus that can be considered a superbug due to its resistance to all types of drug therapy is spreading across the country – with thousands of people already infected, according to health officials.
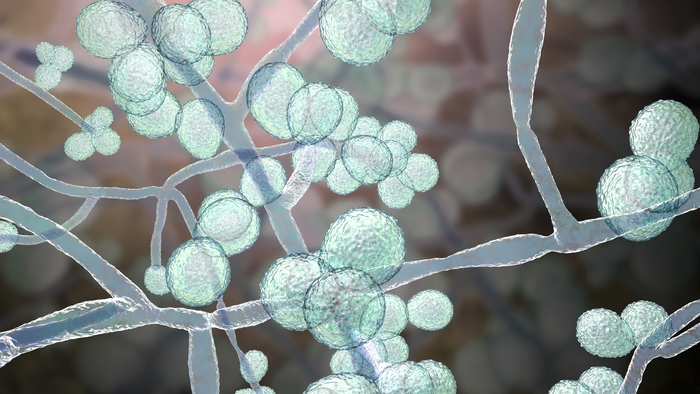
Candida auris, a type of invasive yeast that can cause deadly infections in people with weakened immune systems, has infected at least 7,000 people across 27 U.S. states, according to data from the Centers for Disease Control and Prevention.
The fungus, which can spread easily in healthcare settings such as hospitals and nursing homes, is gaining virulence and spreading at an “alarming” rate, the CDC says.
Some strains of the fungus are particularly troublesome – and even considered a superbug – because they’re resistant to all types of drugs used to treat fungal infections, The Hill reports.
While healthy people may be able to fight off the infection on their own, the fungus can be deadly, especially in healthcare settings, where it can quickly spread amongst a vulnerable population.
“If you get infected with this pathogen that’s resistant to any treatment, there’s no treatment we can give you to help combat it. You’re all on your own,” Melissa Nolan, an assistant professor of epidemiology and biostatistics at the University of South Carolina, told Nexstar.
The fungus’s resistance to drug therapy makes it especially difficult to contain. Currently, more than half of the states have reported clinical cases of Candida auris in 2025, according to CDC data.
Another reason the fungus is such a concern to health officials is that it can survive on surfaces, according to Nolan.
“It’s really good at just being, generally speaking, in the environment,” Nolan explained. “So if you have it on a patient’s bed for example, on the railing, and you go to wipe everything down, if in whatever way maybe a couple of pathogens didn’t get cleared, then they’re becoming resistant. And so over time, they can kind of grow and populate in that hospital environment.”
Candida auris is also dangerous because it can be difficult to identify with standard lab tests.
“The rapid rise and geographic spread of cases is concerning and emphasizes the need for continued surveillance, expanded lab capacity, quicker diagnostic tests, and adherence to proven infection prevention and control,” CDC epidemiologist Dr. Meghan Lyman said in a press release.
The current number of cases, sitting just above 7,000, is fast approaching last year’s record-breaking figure of more than 7,500 cases, according to the report.
A recent study found that Candida auris is gaining virulence and spreading rapidly, not just in the U.S., but also globally.
Candida auris has already been found in at least 61 countries on six continents.
The study also found that the fungus is rapidly becoming resistant to drugs due to its ability to switch from a yeast-like growth form to a filament-driven spread. It also contains a cell wall that has proteins that enable it to stick to human skin “like glue” and colonize it.
“Skin colonisation by C auris is a significant medical concern because colonized patients may facilitate inter- and intra-hospital transmission of C auris to other patients,” the study, published in the Microbiology and Molecular Biology Reviews, says.
The fungus has “efflux pumps” on its cell membrane that can remove antifungal drugs before they can kill it. It also sticks together to form layers on surfaces that makes it more difficult for drugs to penetrate.
It’s unclear if there are any other means by which the fungus resists drugs, the study says. “The diagnosis of C auris infections is often hampered by misidentification, leading to delays in starting appropriate antifungal therapy,” the review explains.
“Taken together, these data underscore the need to develop novel antifungal agents with broad-spectrum activity against human fungal pathogens, to improve diagnostic tests, and to develop immune- and vaccine-based adjunct modalities for the treatment of high-risk patients.”
The study calls for better methods to monitor the fungus, especially in resource-poor countries, as well as greater awareness of the illness.
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks