‘Beyond catastrophic’: How super flu is pushing the NHS to the brink
Leading medics warn of severe hospital overcrowding, staff struck down with flu, and a worrying number of cases among children. Rebecca Thomas reports
In an overrun A&E department, patients line corridors “packed in like sardines” as exhausted medics do their best to avoid falling victim to the “unprecedented” wave of super flu clogging up hospital beds.
Just two weeks before Christmas, top clinicians say this is the worst winter they have seen, with a “flu-nami” driving hospitals to the brink as services face a quadruple threat of winter bugs, an impending doctors’ strike, strict financial demands and patients stuck in hospital beds unable to be discharged into social care.
The sudden and “huge” influx of flu cases – up 55 per cent in the past week – has led health chiefs to fear that overcrowded hospitals will soon be unable to control the spread of infections, leaving vulnerable patients being treated for serious illnesses such as cancer, “terrified” they will catch it.

Dr Vicky Price, president of the Society of Acute Medicine, told The Independent: “It is truly shocking, it is the worst I’ve ever seen it… There are huge numbers of patients lodged in emergency departments, stuck in corridors, in waiting rooms and in inappropriate areas – all very unwell patients, and we’ve got high numbers of staff off sick with flu.
“It’s really concerning, and we have a lot of vulnerable patients, those on immunosuppressants, those who are getting cancer treatment, and they’re terrified to sit in the waiting room, with the systems under strain as it is, there’s nowhere to put these patients.
“We were in crisis anyway with the cold weather, and we noticed a real surge in flu.
“While the ongoing ‘flu-nami’ is being invoked as the primary cause of the crisis, this is a convenient scapegoat when the reality is that the situation is the direct result of a longstanding and predictable breakdown in NHS capacity and workforce shortages.”
Her stark comments come just days after the NHS national medical director, Professor Meghana Pandit, warned that the worst is still to come: “The peak is not in sight yet, so the NHS faces an extremely challenging few weeks ahead,” she said.
It comes as:
- An A&E consultant in North West England said they “don’t have anywhere to see patients… it’s getting to the point where it’s breaking”
- An ambulance chief said their services had seen an “extraordinary” and “unprecedented” number of calls
- A surge in children attending A&E with flu prompts warnings that the infection can have “serious complications” for them
- A pharmacy chief says the delayed rollout of flu jabs is pushing up demand for vaccines too late
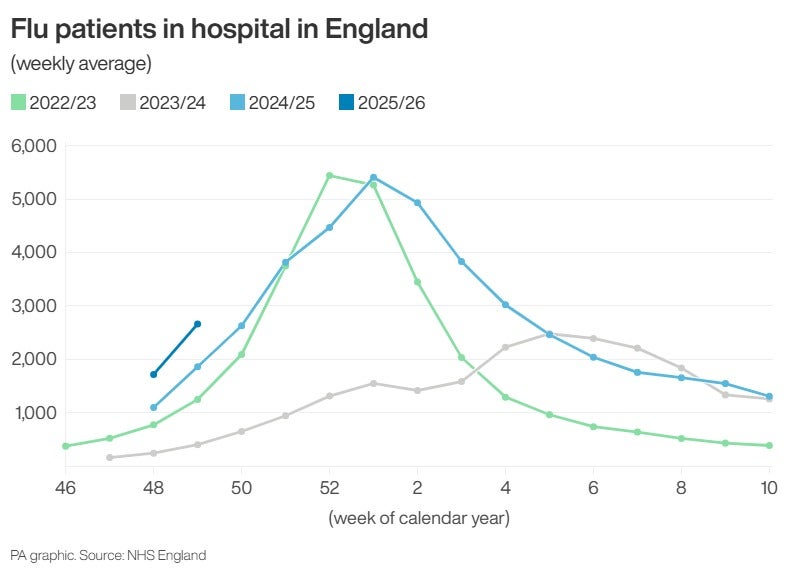
The latest NHS figures show there were 2,660 flu patients in hospital each day last week, while 2.35 million people attended A&Es in November – a record level for that month.
The latest wave has largely been driven by the spread of a new “super” strain of flu, H3N2, which can cause more severe symptoms, and is different from the strain that this year’s vaccines were designed to protect against.
Dr Adrian Boyle, an A&E doctor and past president of the Royal College of Emergency Medicine, told The Independent: “It is crazy busy at the moment, flu is creating a lot of pressure, people are talking a lot about whether fire safety regulation is being breached, because they’re keeping people in corridors.”
Meanwhile, children’s hospitals have also seen a surge in admissions and attendances, and multiple schools across the country have been forced to close to limit the spread of the virus.
Health bosses say that the additional pressures have been compounded by the planned five-day strike by resident doctors due to start on Wednesday, as well as delayed hospital discharges and strict requirements from the government to make financial savings.
One hospital chief in the south of England said: “Pressures come in from about four different angles all at once. Actually, five, if you include the resident doctors’ strike. So the first major pressure we’ve got is the flu. Not just in terms of emergency admissions.
“[It is] one of the worst flu seasons we’ve had, but up until the last few weeks, we hadn’t really been anticipating anything other than a very ordinary flu season… the second pressure we’ve got is delayed discharges, numbers have shot up... [We’re] on the brink of Opal 4, which is our highest level of escalation, which means that we are having to move staff around the hospital to cover staff and gaps, it means that we’ve got beds open that ordinarily we wouldn’t be using.”
The hospital chief said that the third pressure is coming from ambulance services, following national guidance that they leave patients at A&E after 40 minutes so they can get back out on the road.
“The fourth issue we have is that we are under incredible financial constraints, and we’re being told that we’ve got to reduce the amount of banking and agency costs. Then the last one is the resident doctors’ strike.”
Health secretary Wes Streeting has attempted to avert the strike crisis with a new offer to the British Medical Association (BMA), but the doctors’ union is still consulting its members with an answer not expected until Monday – just two days before the planned walkouts.
Mr Streeting said a huge jump in flu cases has left the NHS facing a “challenge unlike any it has seen since the pandemic” and urged resident doctors to accept the government’s offer and end their actions.
The BMA described Mr Streeting’s warnings of a potential NHS collapse as “scaremongering”.
But writing in The Guardian, Sir Keir Starmer said it was “frankly beyond belief” that resident doctors would strike with the NHS under such pressure.
“I am a Labour prime minister, who believes in workers’ right to strike,” said Sir Keir. “But let’s be clear when it comes to the strikes planned by resident doctors next week. They should not happen. They are reckless.”
A No 10 spokesperson demanded doctors’ leaders drop the strikes, warning they will inflict ”pain" on patients as flu cases surge. “NHS colleagues will have to cancel Christmas plans to cover shifts, patients will have operations cancelled, and the NHS will be preparing for the worst in the middle of an unprecedented flu season,” they said.
‘Beyond catastrophic’
There are also concerns about the rapid spread of the virus in hospitals, which is also impacting staff.
Dr Ian Higginson, president of the Royal College of Emergency Medicine, described how patients were “packed together like sardines in corridors”, which meant there is an increased risk of cross-infection.
“Every year, the overcrowding gets worse. So, we’re going into this winter in an absolutely terrible position,” he said.
That threat has prompted South Tyneside and Sunderland NHS Foundation Trust and Frimley Health NHS Foundation Trust to introduce mandatory mask wearing in a bid to slow the spread.
One A&E consultant at a major hospital told The Independent that this was “by far the worst winter that we have had in my time as a consultant”.
They said: “Without a shadow of a doubt, in the last three weeks, it has gone from a bad winter to this is beyond catastrophic. This past weekend, we used every [corridor] space in the trust, and we were holding 71 patients in the emergency department. It’s the worst winter ever. We are rammed in so tight there is no way [to protect against flu].
“We’re told not to test for Covid-19 this year. If we find [Covid in patients], then we have to close beds... the BMA have gone on strike on what will be a horrific weekend. This was not a good moment to call a strike.”
The consultant said tensions inside some overstretched hospitals had reached a boiling point, prompting frustrated patients to target staff.
“We’ve had three assaults on staff since October, the violence against staff has been horrible… doctors who’ve had their faces punched in. Lots and lots of Islamophobia,” they said.
Another consultant in the North West said: “A&E is backed up, [we] don’t have anywhere to see patients, it’s just not fair, quite a lot of respiratory disease… it’s getting to the point where it's breaking. It’s just that awful.”
A consultant in the south of England described similar pressures, saying: “We are beginning this season with tired and worn out staff, no capacity and increasingly less ability to create the temporary escalation spaces – they are already being used most days.
“The main fallacy is that this flu season will tip the NHS into a crisis. We have patients in corridors, both in ED and on the wards, with temporary escalation spaces, usually a chair or a trolley in the corridor. If this is not a crisis, then I don’t know what is. The NHS needs to be honest with itself; it cannot improve if it keeps lying to itself about not being in a crisis.”
Weekly statistics published by NHS England show that around 11,141 patients, 12 per cent, waited in ambulances to be handed over to A&Es – up from 10 per cent last week.
One ambulance chief told The Independent: “It’s pretty self-evident we’ve got huge pressure, we’ve seen an extraordinary number of calls, many patients are waiting in corridors, the flu is causing a major part of that in addition to our pressures.
“The calls [come in with] breathing difficulties because we get a lot of that this time of year, we’ve some unprecedented call volumes.”
Professor Meghana Pandit, NHS national medical director, said: “With record demand for A&E and ambulances and an impending resident doctors strike, this unprecedented wave of super flu is leaving the NHS facing a worst-case scenario for this time of year – with staff being pushed to the limit to keep providing the best possible care for patients.
“NHS staff have pulled out all the stops to vaccinate more people than last year, and with just a week left to ensure maximum immunity from flu for Christmas Day, I would urge anyone eligible for the vaccine to please book an appointment or visit a walk-in site as soon as possible.”
A Department of Health and Social Care spokesperson said: “Flu is a challenge for hospitals every year, and we are under no illusions this is going to be a particularly tough winter for our NHS, which is why we began preparations earlier than ever before and have a plan in place to protect the health service.
“Flu cases are rising, so it is vital that patients and staff can get protected. Over 17 million vaccines have been delivered this autumn – 170,000 more compared to this time last year, with over 60,000 more NHS staff also getting their jab.
“Flu vaccine supplies remain solid, and we would urge everyone eligible to get their vaccination to protect themselves and their loved ones.”
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks