When I went to practice medicine in Australia from the UK, I had no idea what I was getting myself into
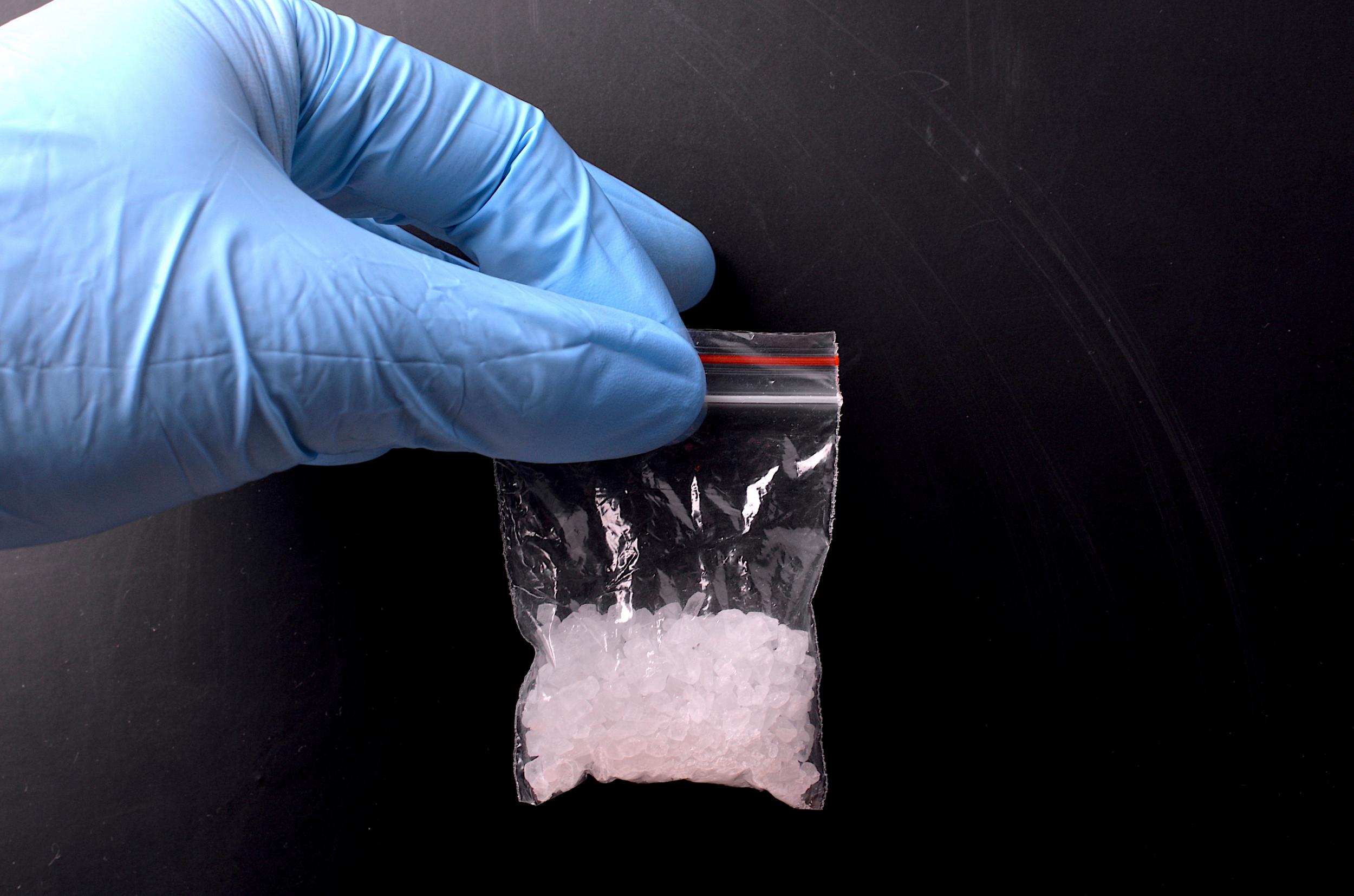
I saw crystal meth decimate Australian hospitals; an epidemic here could stun the NHS
The first time you see someone high on crystal meth, it’s quite a sight. Nobody had really warned me that it was a problem. It was in my first week as an emergency department doctor in one of Australia’s busiest urban hospitals. I saw the young man hurling himself against the walls of the main ward area, sweating gallons, screaming his paranoia to a divided audience of fearful patients and seen-it-all-before A&E staff. Attempts to talk him down ramped him into a rabid rage and before long I thought it only right I help four security staff and a handful of medical and nursing staff restrain his limbs, while bundling the man to the floor before he harmed somebody else or himself. Superhuman strength is overused hyperbole, but this man had it.
As limbs flailed and his squirming form lurched free of his eight captors, he yanked his trousers down and began furiously masturbating. A helpful cleaner tossed a towel into the pantomime. Cubicle curtains were pulled across in prudish haste, to protect our shocked onlookers. I suggested an intramuscular shot of sedative to the careworn consultant, who regarded me as one regards somebody taking a water pistol to a mining town bar brawl. Finally, an intravenous line was passed into the man’s arm and after a doctor administered five times more sedative than I have ever seen given before, the fight was won. Once on a bed we rolled his snoring, inert form on its side, put an oxygen mask on and left him to sleep it off. “You guys don’t really deal with meth in the NHS, do you?”, my Australian boss quipped through a smirk.
For hospital staff in the UK, our only education on “meth” or “ice” is through the cult American drama Breaking Bad. It must stay this way, as a crystal meth problem anywhere near the scale I witnessed daily in Australia could paralyse the NHS.
Though first synthesised in the late 19th century, the first widespread form of the drug was Pervitin, which was distributed to German soldiers to maintain alertness and aggression during the Second World War. This tells you much about its effect profile; historical accounts swing wildly between crediting Pervitin for the Nazis’ astonishing battlefield successes in 1940, to dismissing the drugged storm troopers as hungover zombies. Both seem plausible.
Aside from its devastating potency, meth hangs around in users’ systems for many more hours than most other recreational drugs, stimulating euphoria, alertness and a vigorous sexual drive. It does so by maximising the release of neurotransmitters such as dopamine and serotonin. The comedowns are lengthy and torturous and commonly follow days spent without food or sleep while high. The effects of a binge or, worse still, methamphetamine-induced psychosis can lead to bizarre behaviour, paranoia and violence.
Before I left to practice down under, friends talked about how many snake and spider bites I would treat. I returned feeling I had gained an insight into a very different predator that saps the resources of Australian medicine and society at large and that could make its way to our shores to test the NHS. I will never forget the almost daily struggles to restrain uncontrollably aggressive users. The challenge of inserting an IV line into a fiercely straining, shaking arm pinned by three security or police, egged on by the nursing staff, with the patient screaming that they’re going to kill me. And the unease that if they wriggle free of their tiring captors, they just might.
A couple of cases are particularly imprinted on my memory. One man had been stabbed in the groin during an altercation under the influence of meth. While the team applied pressure to staunch the torrential bleeding from his femoral artery, he began thrashing and fighting wildly to get us away from him. He was a big man, and we were left with no choice but to break away from the bloodbath for our own safety. In many societies, I have no doubt his life would have been left to drain out onto the cubicle floor, while his shouted threats slowly died with him. It would have anyway, were it not for the quick thinking of my consultant that day, who skilfully managed to anaesthetise the patient and allow him to be saved.
Some weeks later, I heard a loud slap from behind a cubicle curtain. I investigated to find a colleague had been hit by a patient in the midst of a meth-induced psychosis. Security were called and I attempted to hold the patient’s arms. It fast became a wrestling match that degenerated onto the department’s floor, as I daren’t let go of him. With security on their way, a collection of assorted A&E staff assembled to watch the writhing spectacle before them, before one sensible soul capped off the farce by wheeling in a portable screen to shield our exertions, and Australia’s shame, from the watching department.

There’s no single reason why we do not currently have a “problem” with crystal meth in the UK. But it is here. It tends to find its place in a small subsection of the urban gay community, where it is taken to fuel lengthy sex parties, known as “chemsex”. Thankfully, it is very expensive compared with other commonly available drugs such as cocaine or heroin and consequently is not seen as a drug of deprivation in the way that it is in Australia and the US. Some have speculated that as a cramped island nation, we lack sufficient open spaces to mass-produce the drug in specialised “meth labs”. Crucially though, anybody with the know-how and access to base ingredients could, in theory, produce modest amounts from the comfort of their own bath tub.
Our almost impossibly resilient health service seems to be able to weather any storm and in the UK we encounter our own issues with drugs and alcohol on a daily basis. However, meth stands alone in its unique ability to grind a department to a halt. The comatose heroin addict is a ubiquitous sight in our A&Es, often floored by an unusually potent new batch. He is wheeled in barely breathing, lifeless hands flopping in early resignation, blank eyes staring to the heavens for oxygen. He poses little threat and requires fewer members of staff to manage than a confused elderly patient, while we assist his breathing and provide antidotes to save his life. A recent emergence of “legal highs” containing cannabinoid and amphetamine derivatives are more unpredictable and disruptive in their effects, though still a far cry from meth’s inimitable potency.
An average A&E shift of doctors or nurses these days is barely able to deal with the normal throughput of patients with their panoply of ailments. Five or six members of staff needing to break off for half an hour to manage a patient high on crystal meth would usher in a new era of chaos and that’s before we even consider its impact during the winter season. While much is made of boozy Britain’s Saturday night carnage in our A&Es, assaults on staff are still relatively infrequent; in certain Australian hospitals, staff assault is increasingly an expected occupational hazard, not the abomination it remains here.
From a moral and legal point of view, both here and in Australia, self-inducement does not in any way alter the level of care we devote to each patient. However, the period immediately following sedation of an aggressive meth user there – normally necessitating massive, anaesthetic-level doses of medication – often made me feel uncomfortable. Normally, with a patient so totally sedated, one would secure their airway and place them on a ventilator, monitoring them at great expense on an intensive care unit bed until they woke. The sheer scale of the problem there often allowed this only in the worst cases, with many users nursed in the recovery position, drooling and breathing shallowly, with no antidote but time. Our NHS is a lesser resourced but more litigious culture – that quite rightly implores the highest standards for all – and our intensive care units would also bear the brunt of urban outbreaks of meth supply.
I am, of course, only envisaging the burden it would impose on emergency and acute medical services. The many long-term mental, physical and social effects are a further depressing study of dependence and decay. The famed “meth mouth” – the tell-tale bleeding gums and brown, broken-toothed grimace of the seasoned user, is an apt metaphor for the societal decay the drug can wreak in badly affected regions.
Of course, there are many imminent threats to the health service without scaremongering and “what ifs”. There is so little time to draw breath every April, following the winter onslaught that annually seems to grip ever more of autumn before and spring after, that foresight seems a scarcely affordable luxury. However, having experienced at first hand the demonic whirlpool of destruction generated by crystal meth, it is clear we must anticipate the threat of its growth head on. When it has brought far better resourced systems almost to their knees, medics and policy-makers must fear the cold blast from “ice” in the same way we would dread a permanent winter crisis.
Sam Goodhand is a doctor in anaesthesia and critical care
Join our commenting forum
Join thought-provoking conversations, follow other Independent readers and see their replies
Comments
Bookmark popover
Removed from bookmarks